In an interview conducted by Dr. Damon Adams, Dentistry Today’s Editor-in-Chief, Dr. Michael Tischler maintains a private practice in Woodstock, NY.
Dr. Adams: As a general dentist, how have you incorporated dental implant surgery and prosthetics into your practice so successfully?
|
|
||
|
Dr. Tischler: It starts with a strong belief that dental implants are the ideal way to replace missing teeth. If you look at the literature comparing the other options available to replace missing teeth; a fixed tooth borne prosthesis, a removable appliance, or a bonded fixed prosthesis; dental implants offer the best long-term success without being a detriment to adjacent teeth. At the same time, according to the literature, dental implants preserve or stimulate bone. This information was first brought to my attention years ago by Dr. Carl Misch, and I am so grateful for his mentorship and training throughout the years through his institute. Once you really understand that dental implants best recreate natural tooth function in edentulous regions for both partially and fully edentulous areas, you just want to convey this to your patients.
Overall, I believe that the success rate with dental implants I experience in my practice is related to the principles of treatment planning that translate to favorable loading forces on implants. When dental implants can be treatment planned so that their placement positions do not create undue occlusal forces and angulations, there is less bone loss, and prosthetic breakdown. My friend Dr. Scott Ganz has said that, “patients come to us for teeth not implants.” I like that quote because that is how I treatment plan, from the prosthetic end result backwards. Once you decide with the patient what the end result will be, you can then plan a case by looking at the bone levels and soft tissue architecture. This is the foundation for implant dentistry.
From a practice management standpoint, successful incorporation of implants into my practice has been facilitated through good marketing and staff support. My Web site tischlerdental.com has a lot of information about dental implants that many patients utilize. My team is totally on board with the clinical benefits of dental implants and they convey that message to our patients on a daily basis in person and on the phone.
|
Dr. Adams: What is new and exciting in the field of implant dentistry?
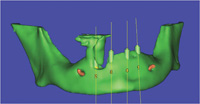
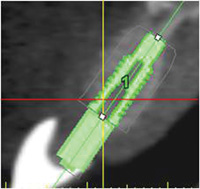
Dr. Tischler: The utilization of cone beam computed tomography (CBCT) is, in my opinion, the most dramatic influence and exciting thing happening right now. The technology that CBCT offers, allows for a dramatic increase in safety, and predictability in implant treatment planning. In my office I have an iCAT CBCT machine, and for the past 2 years, I have not placed a dental implant without using it. There is no other way to get 4 views of a jaw including a 3-dimentional (3-D) view. I can outline the mandibular nerve, visualize bone density, sinus anatomy, and any potential pathologies, as well as many other parameters. Once I plan the location of implants to be placed, I can have a surgical guide created that accurately translates to the mouth, the correct location, angulations and depth for implant placement.
The most recent development in the CBCT field is the formation of third-party companies such as 360 Imaging in Atlanta that process and treatment-plan the information from a CBCT and allow for an online meeting between the surgical and restorative doctors. This is first time, in my view, that the team approach between all doctors involved with a patient’s treatment can easily be coordinated and communicated in an effective manner. This now allows the restorative doctor to help guide the surgeon based on a prosthetic end result. This now allows dialogue between treatment doctors and a realistic and powerful team approach.
In general, I believe the predictability that CBCT offers will allow the number of dental implants placed to increase and to help the many patients out there that need it.
Dr. Adams: Should general dentists place dental implants?
Dr. Tischler: Implant dentistry is not an ADA-recognized specialty. In this country, a licensed dentist can surgically place dental implants as long as they abide by the standard of care for dental implant placement. Dental implant surgery is not generally taught in dental school so a graduating dentist must learn this standard of care through postgraduate educational venues.
The path I took for this was a conglomerate of what I feel are some of the best educational venues in this country by practitioners that are willing to share their knowledge about implant surgery and prosthetics. The Misch Institute is based on the teachings of Dr. Carl Misch, the author of the best selling textbook in the world on implant dentistry. The fundamental principles taught there, and the availability to bring your own patients, is a great opportunity to learn. The instructors at the institute are there to guide you during your first few surgeries, increasing your confidence as you start out. This was powerful for me. Supplementing that with other surgical courses that are available, such as Dr. Mike Pikos’s MAP Institute in Florida, Dr. Pat Allen’s soft tissue course in Dallas, and Drs. Salama and Garber’s courses in Atlanta, were also part of my educational journey. There are also many university-based programs that offer surgic
al guidance. A dentist can attend as many courses as they want but at some point they are going to have to get in the mouth and start actually placing implants so they can build their comfort level and skill levels.
I also feel it is important to join some of the major implant organizations and get involved. The International Congress of Oral Implantologists, the American Academy of Implant Dentistry, the Academy of Osteointegration offer great educational venues, annual meetings and periodicals to stay abreast in the field of implant dentistry. While the credentials these organizations offer, give a practitioner something to hang on their wall, the real value in the credentials are the process that it takes to get them. The American Board of Oral Implantology Implant Dentistry offers a board-certification process that I have completed. This process, offers a similar testing protocol that board certification requires for other dental specialties. Just the vigor’s of this exam and preparing for it, I feel brings a doctor to a higher level of care. One other thing I recommend is for general dentists to join the American Academy of Periodontology (AAP) as an associate member. A sponsorship is needed by a periodontist who is an AAP member to join. The AAP’s Journal of Periodontology and the annual meetings offer excellent information on implants and grafting.
|
Dr. Adams: You have stated in your lectures and articles that fixed implant dentistry is easier than crown and bridge on natural teeth. Can you explain this?
Dr. Tischler: The steps involved in taking an impression, and having the laboratory perform the needed steps to deliver a final fixed prosthesis, is less labor intensive and equally predictable as a tooth-borne crown and bridge impression. I often say that to perform fixed implant prosthetics, a dentist has to be good at screwing and unscrewing parts, and taking impressions. Any dentist can do that! The dental laboratory technicians really do a majority of the work in the lab. They prepare or create an abutment, create provisionals, and can order all parts and pieces needed. The dental lab is actually an integral partner in the implant team.
The fact is that since most dentists don’t understand the parts and pieces involved it becomes intimidating. When you don’t understand something you tend to shy away from it. It is a shame because the literature supports the fact that a single tooth implant has better longevity than a 3-unit bridge, and it is easier to clean for the patient, puts less stress on adjacent teeth, and stimulates the bone.
I do believe for the entire process to be predictable and simplified for the restorative dentist, the surgeon must create the correct hard and soft tissue support for this to happen. Unless an implant is relatively parallel, in the correct position form an occlusion and aesthetic standpoint and the soft tissue is healthy, the process to restore an implant is made more difficult. This is why the restorative dentist must get involved in the process to make sure that in the end, the prosthesis is correctly supported by the implant. It all comes down to correct treatment planning. Also, the importance of bone grafting for success of the final prosthesis cannot be overemphasized. Correct bone levels will dictate the implant to crown ratio, papillae support, and angulations of implants. These are real issues that define the long-term success of a case. This is why I emphasize bone-grafting principles in my courses.
Dr. Adams: With so many implant companies and products available, how do you choose what to use?
Dr. Tischler: It is amazing how many implant companies you see in the journals and at meetings. For example, at the 2008 Greater New York Dental Meeting, there were many implant companies and implant related products to see there. There is an obvious increase in their presence, and this is encouraging since the meeting is mostly a general dental-based meeting. This is certainly a sign of where the implant market is going, as it should. The amount of edentulism in this country is high and people are living longer. The bottom line is that a dental implant offers the best alternative to replace missing teeth and as dentists we can offer that opportunity to our patients.
A clinician really needs to set apart marketing hype from the science of what a product offers. Doing this requires a little research and knowledge of what an implant offers in design for instance, or what a membrane offers to the surrounding tissue and how it handles. For instance the implant I have used for the past 10 years is made by BioHorizons. I like the fact that they have a square-shaped thread that allows for increased surface area and that it also comes with a stock abutment, which can be used much of the time. Each implant company offers different design features and nuances that make their product unique. It is up to the clinician to research products and decide what works best for them.
Dr. Adams: How do you get your patients to accept treatment plans which include implants with the associated higher fees?
Dr. Tischler: I start with the awareness that a large portion of the US adult population is missing teeth. I am also knowledgeable that dental implants are the best way to replace missing teeth. Understanding these 2 facts, I basically present what is ideal with respect to implant treatment and accept the percentage of people that can find a way to afford this higher level of care.
I also present alternative plans for patients with regards to implant plans. Often alternative plans include building towards
ideal plans with removable implant supported appliances. Over time these removable implant supported appliances can be converted to a fixed prosthesis with additional implants being added for support. In my practice I offer the services of various finance companies such as Capital One and CareCredit, to assist my patients. These financial companies allow me to offer financing without personally taking a risk. I feel the administrative fees these companies charge are outweighed by the convenience to the patient and increased acceptance of plans we see.
When it comes to a patient actually accepting implant treatment recommended, it is directly related to the clinician’s confidence in their plan and conviction that what they are presenting is right for the patient. A patient makes large decisions such as an implant treatment plan based on many factors. These factors include, trust in the clinician, the reputation of the practice, feeling comfortable in a dental facility, the marketing and website they have seen, communications from the doctor and staff, and more. It is not just one thing that seals the deal.
In the end I feel the overriding driving factor is a clinician’s commitment to ideal care from dental implants for their patients that drives the many factors involved with creating a successful implant practice. That belief system will energize many things to happen. Unless the clinicians educate themselves or experience the benefits of dental implant services, it will be difficult to convey this with conviction.
Dr. Adams: Why is bone grafting such an important topic for you?
|
Dr. Tischler: The importance of bone in relationship to the final dental implant prosthesis cannot be overemphasized. It is imperative for any clinician involved with dental implants to understand that unless bone is in a position to support a dental implant, the implant to crown ratio, implant aesthetics, soft tissue around implants, occlusal position, and implant angulation will be affected. These are the most important aspects related to the success of implant treatment.
The status of bone supporting a dental implant should be considered during the treatment planning phase. This can be best done through utilizing CT. To place an implant in a compromised position because “the bone is there” is not justified. The present bone grafting science allows for highly predictable growth of bone. Once a prosthetic end result is determined, bone can be grafted to fulfill that desired position. General dentists extract around 22 million teeth a year according to a recent ADA survey. It has been extrapolated in the literature that only 2% of extraction sites are being grafted. General dentists are not grafting extraction sites. Also in the literature over and over again, it has been proven that once a tooth is extracted, a patient will lose bone in both height and width. Through grafting an extraction site, the bone can be preserved for future implant placement or at least for pontic site development.
Whenever I lecture on dental implants, I include information on bone grafting because of the integral relationship that exists. It is a package deal between understanding dental implant science and bone grafting. They cannot be separated. I would even go one step further that to really tie everything together, soft tissue fundamental principles also need to be understood. What good is a dental implant without healthy surrounding soft tissue? This becomes even more crucial in the aesthetic zone with reference to correct papillae formation since bone supports the soft tissue. I feel that any adjunctive knowledge related to dental implant treatment is important in order to tie it all together and create implant treatment success. Implant dentistry in general, is a multidisciplinary treatment modality. The disciplines involved include biomechanics, pharmacology, cosmetic dentistry, radiology, prosthetic dentistry, anatomy, physiology, and psychology. Psychology might be one of the most important especially when you deal with larger cases that require patient compliance over a long period of time.
One more area of bone grafting that is important for every dentist to understand is sinus grafting. With the posterior maxilla often edentulous because of greater forces and weaker bone, it is important for dentists to know that this region can be predictably augmented for placement of dental implants. This can be performed through various techniques, but in the end a patient has an implant supported prosthesis that outperforms a removable prosthesis on every level. Why shouldn’t a dentist let their patient know this fact? This is just another example of why every dentist should understand the science of implant dentistry and bone grafting.
Dr. Adams: What are your recommendations to your fellow general dentist colleagues with regards to implementing implant dental procedures in their practice?
Dr. Tischler: Considering the substantiated need for dental implant services and future growth of implants in the dental industry, every general dentist should have a firm grasp of this discipline. The increase in needed implant services in the future is only going to increase. I strongly recommend for every clinician to embrace this discipline, even if only to be able to converse intelligently with his or her patients. For colleagues that wish to further their involvement in implant surgery, start with introductory courses to get the ball rolling. Build a foundation from the ground up and find your comfort level. Take courses that allow you to do actual surgical procedures under the guise of experts. If you choose as a general dentist to take on surgery, then allow at least a year or so to build the needed skills and when you are ready start with simple procedures in your practice. It is a multidisciplinary area of dentistry and the learning curve is steep. If you respect that, and are patient, it will happen.
Get involved with implant organizations, study groups, and respected training programs. Get your staff involved as well, because they can carry your message. Realize that whatever you do will be held up to the standard of care in the profession, so make sure you dot every i and cross every t. One of the most important things to do as an implant restorative dentist is to communicate with your surgeon clearly and your laboratory clearl
y and build a team approach. Enjoy every aspect of implant treatment, but be prepared to deal with problems that will arise. Relish the opportunity to provide such an outstanding service for your patients and be ready to enter a whole new world of dentistry.
Dr. Michael Tischler is a general dentist in private practice in Woodstock, NY. He is a Diplomate of the American Board of Oral Implantology Implant Dentistry, a Diplomate and Fellow of the International Congress of Oral Implantologists, a Fellow of the American Academy of Implant Dentistry, and a Fellow and graduate of the Misch International Institute. He is on the Dental Advisory Board for Dentistry Today and on the Editorial Advisory Board for the Journal of Implant and Advanced Clinical Dentistry. He has published many articles in various dental journals and lectures internationally on the principles of implant dentistry and bone grafting. He is the director of implant education for Microdental Laboratories and is also on the Biohorizons educational speaker’s panel. He offers in-office courses at his teaching facility in Woodstock many times during the year and has a popular instructional DVD available that covers the principles of implant dentistry and bone grafting. He can be reached at (845) 679-3706 or by visiting tischlerdental.com.
Disclosure: Dr. Tischler receives and honorarium as an educator presenting for BioHorizons.