When the dental profession started to use composite resins, there was only one type of material: large particle size composite. Since then, dentists have been bombarded by the terms: macrofilled, fine-particle resin composites, microfilled, hybrid, microhybrid, nanofilled, nanohybrid, and now, nanodimer. What does all of this mean and what does a dentist need to know about these categories of composite resin materials in order to practice everyday dentistry with success?
Do these different categories have benefits that should lead us to use one over another? Are we behind times if we do not use the newest one? Are we selecting clinical materials using incorrect criteria? What else is important from a clinical perspective for everyday success? These are the questions that will be addressed in this article. In lieu of a written case report, a step-by-step technical demonstration will also be shared, showing the author’s techniques for placing a composite resin restoration.
HISTORICAL PERSPECTIVE
An ultimate goal of adhesive dentistry and composite resin restorations is to have a material that is dimensionally and chemically stable, with the ability to seal the restoration without micro or nanoleakage at the margins of the restoration. To date, this has not been completely achieved. This is because in order to obtain superior properties, other properties have to be compromised. However, clinical techniques have been developed to manage some of the complications, such as the layering technique which helps to overcome shrinkage.
In general, the evolution of resin composite technology has progressed from large particle size inorganic filler particle composite resin products to smaller particle size configurations with enhanced fillers. This progression has resulted in composite resins that are smoother and stronger, and have produced less shrinkage during polymerization.
 |
 |
|
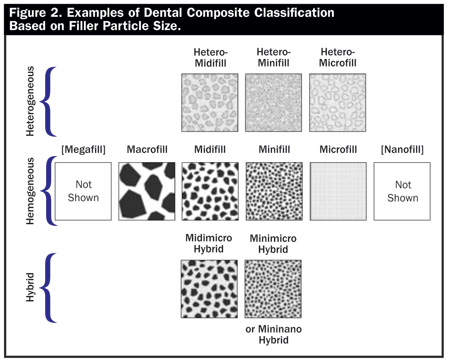
Figures 1 and 2. Resin composites can be arranged by filler particle size. Figures 1 and 2 show this relationship first in a linear display, and secondly by relative size and distribution of the filler particles in the resin matrix. Dental Materials. In: Roberson T, Heymann HO, Swift EJ, ed. Sturdevant’s Art and Science of Operative Dentistry, 4th ed. New York, NY: Mosby; 2001:195-196. Adapted with permission from Elsevier. |
Resin composites can be arranged by filler particle size (Figures 1 and 2). Nanofills (ie, Filtek Supreme [3M ESPE]) contain the smallest particles while macrofills (ie, one of the early composites called Concise [3M ESPE]) have the largest. Most recently, manufacturers and researchers have come to the conclusion that the best composite resins should ideally consist of micron (µm) sized particles combined with nano-sized particles to provide high strength, less shrinkage, high polishability, and better optical properties. Further enhancements have been recently made by adding nanofibers to optimize the restorative aesthetic abilities of these materials (ie, Tetric EvoCeram, Ivoclar Vivadent).
|
- strength
- polymerization depth and time
- ambient light sensitivity
- radiopacity
- shrinkage
- wear
- handling (sculptability, stickiness, stiffness)
- modulus of elasticity (flexibility)
- physical properties (hue, value, chroma, translucency, fluorescence, opacity, polishability)
- clinical longevity
- the product’s indications and contraindications for use.
As new products are launched, sometimes a superior claim is made about the product in one category or another. However, most of the time, another property is compromised in order to produce the identified superior feature. There are multiple examples of such products that come and go. For example, a new composite resin may claim superior low shrinkage as compared to other products, but when curing times are reviewed, that product may require twice as long (or longer) to cure. Another example would be a product that advertises excellent wear resistance but sets too fast in ambient light thus providing the dentist insufficient time for placement. At times, a composite may have excellent physical properties but its shades are not matched to the included shade guide. A product may have excellent depth of cure, but wears too fast or is too brittle. Therefore, it is important to understand properties that result in clinical success, and also understand a material’s limitations so that a dentist can modify clinical techniques to overcome the shortcomings. For example, we have been working with composite resin systems with relatively high polymerization shrinkage (between 3% and 5%) for a considerable amount of time, but with reasonable clinical results (ie, Esthet-X [DENTSPLY Caulk]).
It is critically important for today’s dentist to read and become familiar with the chemistry and a product’s instructions or directions for use (DFU). This is also important for all team members (staff) who may be assisting with, or using a product clinically. Even a minor misunderstanding concerning the recommended polymerization steps of adhesive application can have irreversible consequences for the success of the restoration. Besides these clinical concerns, dentists should take time to inquire about the in vitro and in vivo test results supporting the product and/or its specific claims. Dentists must also question the test protocol of the product’s research studies and ask how long was the product tested.
One of the “truisms” in dental product selection is to know how long a product has been on the market and how successful have dentists been with its use? (What are the parameters for success and has it been documented properly?) There are products that have been on the market for several decades (ie, Heliomolar [Ivoclar Vivadent] and Herculite [Kerr]) and yet these materials (or newer versions) continue to be produced and used successfully. If one was to review the characteristics of these 2 products to the above listing of attributes, it would become apparent that they continue to rank very favorably. It is fortunate for dentists to have products such as these because as a product is used over time, familiarity with the product increases, and through correct repeated usage more clinical success is achieved.
What are “Musts” and What are “Nice to Haves” in Material Se
lection?
Minimally the “musts” should include:
- high compressive strength and adequate wear resistance
- low shrinkage
- good depth of cure
- low ambient light sensitivity
- color stability
- good handling characteristic
- adequate translucency, fluorescence, opalescence, and opacity
- polishability and polish longevity
- radiopacity
The above listed characteristics are important considerations when selecting resin composite products. The more a specific product can be highly rated concerning these properties, the more it can demonstrate clinical success. Today’s dentists have to be chemists plus mechanical engineers in assessing dental bio materials. Success and failures are determined by physical properties, and how a product is utilized. Most dental manufacturers have Web sites that describe their products. Dentists can visit these Web sites to review a product’s attributes and the research that support its claims. Additionally, the Web sites contain recommended DFU and instructional videos. By having these sources of information, dentists can practice with the necessary knowledge to produce the best restorations.
CONCLUSION
In conclusion, there are many different resin composite materials available today for the dental profession. A dentist must have an understanding of what makes one resin composite material perform better than others. Features such as compressive strength, shrinkage, and wear are critical for clinical success. Sometimes advertisement claims will steer the dentist to a certain product primarily based on one superior attribute without a clear understanding that the product may have deficiencies in major properties that can compromise clinical outcomes.
In addition, one must know how to handle a particular composite resin system clinically. This entails employing the right instruments and being up-to-date on the current methods for proper placement. (See the Sidebar demonstrating the author’s step-by-step technique for proper clinical placement using one example of a contemporary composite resin system.)
By having an awareness of any material strengths and weaknesses, and understanding the proper clinical steps and techniques, dentists will be better informed and can become empowered to make informed choices.
Dr. Antonson received his DDS degree from Loyola University, Chicago, and his Master’s Degree in Education from the University of Florida. He has been voted Teacher of the Year on several occasions and honored by President Gerald Ford for his service to the profession. He is a member of Omicron Kappa Upsilon, both the American and International Colleges of Dentists, the International Association of Dental Facial Esthetics, and vice chairman of the World Federation of Laser Dentistry, North American and Canadian Division. Currently, he is professor and associate chair, Department of Restorative Dentistry at the College of Dental Medicine, University at Buffalo, SUNY. His research interests include adhesive dentistry, microconservative dentistry, cariology, remineralization, dental lasers, periodontal/ restorative relationships, polymerization techniques, indirect restoration techniques, ergonomics, CAD/CAM, and ceramic-based restorations. His basic philosophy of minimally invasive dentistry predicates all of his treatment and teaching recommendations. He has given more than 200 national and international presentations as well as being published in texts, teaching manuals, research abstracts, articles, and book chapters. He can be reached at (716) 829-6361 or antonson@buffalo.edu.
Disclosure: Dr. Antonson reports no conflict of interest.

















