Over the years, practitioners have reported frustration when the fit of a removable partial denture framework at try-in does not coincide with the fit at insertion. Clinical techniques in making impressions, making a master cast, making a framework, and processing resin are factors that must be reviewed when considering possible causes for unacceptable clinical results. Reducing potential errors throughout clinical and laboratory procedures can benefit the quality of the final prosthesis, as well as the fit at insertion.
After clinical verification at metal framework try-in and acceptance of occlusion, laboratory factors such as flasking, compression molding, and devesting are suspect in creating deformation of the various components, such as minor connectors and major connector of the framework. Deformation of framework components can be overlooked unintentionally and can be a complicating factor resulting in improper fit at clinical insertion of the prosthesis. Even after customary adjustment of the resin base material, it may be determined that the removable partial denture does not seat properly. In a more drastic situation, such as removal of all resin material from tissue-bearing areas, which still results in the framework not seating completely, it is highly suggestive that deformation of the metal framework has occurred after processing in conjunction with other lab procedures.
This article will follow the care of a patient requiring a maxillary complete denture and a mandibular removable partial denture, and will highlight the technical steps utilizing a flaskless process in removable partial denture fabrication.
AVAILABLE PROCESSING TECHNIQUES
Denture base resins are processed through various techniques in an effort to achieve as accurately fitting a prosthesis as possible. These materials have limitations, and certain techniques have been developed to help overcome some of these limitations. These various techniques utilize the following to create the final prosthesis: denture resin shaped via compression molding; injection molding; gravity pouring (fluid flow into a vented mold); or physical pressing and shaping of the resin onto a master cast in free space.
Whatever the technique utilized, denture base resins undergo polymerization changes as free radicals are generated by heat and/or light and/or chemical reaction. External and internal heat of polymerization activate the crystallization process. External heat sources include variable temperature water baths (with or without pressure), microwave energy, or light energy.
Denture base molds generally consist of paired chambers allowing resin to be introduced directly into open mold halves that are then pressed together, or the resin is introduced indirectly through a sprueway into closed mold halves. Direct introduction of resin into open mold halves requires a resin with doughy consistency (medium viscosity) to undergo compression shaping as the halves are closed. Introduction of resin through a sprueway requires a resin with somewhat lighter viscosity properties to create a uniform flow when injected into the closed mold cavity. The resin may be highly fluid (extralight viscosity) and poured through a sprueway, in which case multiple sprues and a vent are required.
Both compression molding and injection molding require rigid mold forms to resist distortion during introduction of the resin. Pouring offers the opportunity to use flexible mold materials–generally hydrocolloid and silicone materials–which allow easy devesting and recovery of the processed, anatomically shaped prosthesis.
Regardless of the technique employed, the quality of the prosthesis may vary according to the material used and the skill of the operator. It is generally agreed that all these techniques can provide clinically acceptable outcomes. The question of which technique consistently produces the required result is under ongoing investigation.
The purpose of this article is to direct the reader to evaluate a method utilizing the shaping of denture base resins by pressing heat-softened resins directly onto the master cast and framework, thus eliminating the need for an anatomical wax-up and flasking procedure. These types of resins have working properties similar to waxes, allowing shaping of the denture base resins and denture tooth arrangement, permitting trial insertion prior to processing in free space. This direct resin system is a unique technique that provides for a wax-free, flaskless method for fabrication of removable prostheses. The ability to process denture base resins onto a cast removable partial denture framework without flasking and devesting helps eliminate or minimize the possibility of errors in flask closure and removable partial denture framework distortion that can occur during devesting.
MATERIAL
The material presently used in this technique is a light/heat-cured methacrylate (Eclipse Prosthodontic Resin [DENTSPLY Prosthetics]). There is no vaporizing monomer, which is an advantage of this material. This resin does not chemically bond to acrylic teeth. However, an extremely strong bond is achieved using a bonding agent that enables reactive methacrylate-terminated dimers and oligomers to diffuse into the surface structure of an acrylic denture tooth.
The recommended bonding agent is reported to provide excellent bond strength between the resin and the denture teeth. Additional mechanical augmentation can be created by placing diatorics into the denture teeth. Even though this is not required by the manufacturer, the additional mechanical retention gained and increased surface area for bonding is worthy of consideration. The reader should be aware that a large diatoric can weaken the denture tooth, so if modification of the denture tooth is prescribed, it should be conservative. The bonding agent reacts through the use of a solvent vehicle that encourages penetration of the oligomers into the denture teeth. Reactive entities, once initiated, undergo additional polymerization, predictably bonding the teeth to the denture base.
PATIENT TREATMENT
A 76-year-old female patient presented with a loose, ill-fitting maxillary complete denture and a poorly adapted mandibular removable partial denture. The mandibular removable partial denture was a Kennedy class I with a bilateral distal extension and showed a “stepped” plane of occlusion between the natural dentition and the RPD occlusal plane (Figures 1 and 2).
 |
| Figure 1. Frontal view of patient with a maxillary complete denture and a Kennedy class I removable partial denture. |
 |
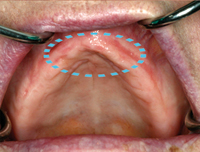 |
| Figure 2. Frontal view of patient showing the mandibular occlusal plane discrepancy between the 6 anterior teeth and the posterior denture teeth; appears as a “step” transition when the denture teeth wear over a period of use. | Figure 3. View of the edentulous maxilla. Highlighted area is the premaxilla surgical site. |
Intraoral examination revealed generalized maxillary bony resorption coupled with excessive premaxillary resorption (Combination Syndrome; Figure 3). The man-dibular arch contained teeth Nos. 21 through 28, and the remaining bilateral posterior edentulous areas were adequate for the fabrication of a new removable partial denture, even though it was evident that alveolar bone resorption had occurred. In an effort to preserve the remaining premaxilla from further deterioration, it was decided to correct the occlusal plane, thereby transferring functional loads to the posterior bearing areas.
The following outline provides an overview of the treatment rendered to this patient:
(1) Surgical modification of the premaxillary redundant tissue with nasal spine refinement.
(2) Fabrication of a new maxillary complete denture restoring the appropriate plane of occlusion.
(3) Fabrication of metal ceramic crowns on tooth Nos. 21 and 28 to facilitate correction of the mandibular occlusal plane. It should be noted that the patient declined the more conservative treatment option of enameloplasty of remaining mandibular teeth.
(4) Fabrication of a new mandibular removable partial denture with appropriate coverage of all key anatomical areas such as the retromolar pad and bilateral buccal shelf areas, restoring the patient to the appropriate occlusal plane.
Treatment Sequence
 |
| Figure 4a. View of the previous prostheses; the frontal view demonstrates the inverted curve in the anterior area. | Figure 4b. A duplicate maxillary denture was made and an occlusal splint was incorporated into the transitional prostheses to allow the patient to accommodate to the improved occlusal plane. | Figure 4c. View of the new prostheses and the correct plane of occlusion. |
 |
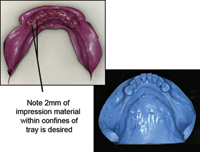 |
| Figure 5. View of the maxillary master impression showing use of multiple viscosities of polyvinyl siloxane impression material, and view of the maxillary master cast made from master final impression (Aquasil Ultra PVS [DENTSPLY Caulk]). | Figure 6. View of the mandibular master impression using a medium-bodied viscosity polyvinyl siloxane impression material, and view of the mandibular cast made from master final impression (Aquasil Ultra PVS [DENTSPLY Caulk]). |
 |
 |
| Figure 7. View of the mandibular arch with new removable partial denture in position intraorally. Pictured right is the frontal view of the completed prostheses. The final occlusion developed for this patient shows a reverse occlusion in the posterior areas. | Figure 8. Frontal view of the patient’s lip posture with the previous prostheses; note the reverse posture of the lips in repose. |
 |
 |
| Figure 9. Frontal view of the patient with the new prostheses with re-establishment of an acceptable nose-lip-chin posture. | Figure 10. Left, view of the patient’s profile with the previous prostheses. Right, view of the patient’s profile with the new prostheses. |
 |
 |
| Figure 11. Frontal view of the patient with previous prostheses before treatment. | Figure 12. Frontal view of the patient with new prostheses after treatment. |
The clinical procedures for fabrication of the prostheses were initiated after completion of preprosthetic surgical procedures and appropriate healing time had passed. A duplicate maxillary complete denture was fabricated; the duplicate denture allows for aggressive alteration of the prosthesis to fit the proposed occlusal scheme and creation of an occlusal splint to allow the patient to accommodate to the proposed occlusal plane (Figures 4a to 6). Procedures were completed to fabricate metal ceramic crowns on teeth Nos. 21 and 28. During the fabrication procedures, each wax pattern was surveyed and waxed to incorporate guide planes and rest seats as well as verification of the design in the final metal ceramic restorations. After metal framework try-in and jaw relation record verification, resin polymerization was initiated. The mandibular removable partial denture was then seated opposing the new maxillary complete denture. Necessary occlusal and intaglio adjustments were made (Figures 7 to 12).
Postinsertion instructions were reviewed with the patient, and then the patient was appointed for a 1-week follow-up appointment. Minor adjustments were completed. Both the maxillary complete denture and the mandibular removable partial denture were inspected at 1-, 3-, and 6-week intervals without additional need for modification. The patient was then scheduled for routine follow-up appointments.
 |
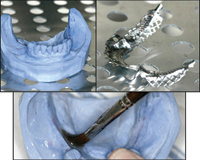 |
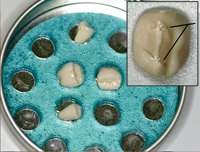
| Figure 13. The denture teeth are placed, ridgelap down, into a warm solution of bonding agent for 1 to 5 minutes to coat the contact surface and ensure final bond. In upper right insert, a conservative diatoric was created on the ridgelap surface of the denture tooth. | Figure 14. Both the mandibular master cast and the mandibular removable partial denture framework are heated in preparation for making the final prosthesis. A releasing agent is applied to coat the mandibular master cast prior to adapting the denture base resin. |
 |
 |
| Figure 15. The resin (Eclipse baseplate resin) is heated following manufacturer fabrication instructions. Pictured right: adapt the resin onto edentulous areas of the master cast by compressing the material firmly. | Figure 16. After adapting the initial layer of resin, place the framework on the master cast and press into position as judged by adaptation to the teeth and other anatomical landmarks. Next, additional resin application and shaping can be accomplished using the thermal-controlled air gun to approximate appropriate anatomical form. |
 |
 |
| Figure 17. The denture teeth can be set into the resin material and fixed into position using additional resin between the tooth and denture base material. Use a heated instrument to refine cervical and interproximal contours. Pictured right, occlusal view of the denture teeth positioned in the mandibular removable partial denture. | Figure 18. As the denture teeth are positioned, the occlusion is verified in the articulator, and any adjustments are accomplished. The prescribed occlusal vertical dimension is verified on the articulator. |
The laboratory procedures followed in this flaskless technique for fabricating the mandibular removable partial denture are shown in Figures 13 through 18. The process highlighted for this patient’s treatment began after the removable partial denture framework had been made following an accurate master impression technique and the metal framework fit was verified clinically.
CONCLUSION
A technique has been described that utilizes the shaping of denture base resins by pressing heat-softened resins directly onto the master cast and framework, thus eliminating the need for an anatomical wax-up and flasking procedure.
Sources
Kelly E. Changes caused by a mandibular removable partial denture opposing a maxillary complete denture. J Prosthet Dent. 2003;90:213-219.
Palmer BL, Coffey KW. Investing and packing removable partial denture bases to minimize vertical processing error. J Prosthet Dent. 1986;56:123-124.
Palmqvist S, Carlsson GE, Owall B. The combination syndrome: a literature review. J Prosthet Dent. 2003;90:270-275.
Rudd RW, Rudd KD. A review of 243 errors possible during the fabrication of a removable partial denture: part I. J Prosthet Dent. 2001;86:251-261.
Rudd RW, Rudd KD. A review of 243 errors possible during the fabrication of a removable partial denture: part II. J Prosthet Dent. 2001;86:262-276.
Rudd RW, Rudd KD. A review of 243 errors possible during the fabrication of a removable partial denture: part III. J Prosthet Dent. 2001;86:277-288.
Tanoue N, Nagano K, Matsumura H. Use of a light-polymerized composite removable partial denture base for a patient hypersensitive to poly(methyl methacrylate), polysulfone, and polycarbonate: a clinical report. J Prosthet Dent. 2005;93:17-20.
Dr. Massad is adjunct associate faculty, Tufts University School of Dental Medicine and adjunct associate faculty, Department of Prosthodontics, University of Texas Health Science Center, San Antonio. He has published articles in the Journal of Prosthetic Dentistry, International Journal of Periodontal and Restorative Dentistry, Compendium of Continuing Dental Education, The In-dependent Journal England, The Pankey Gram, Bulletin of American Association of Dental Examiners, Journal of the Oklahoma Dental Association, Dentistry Today, Dental Economics, and others. He can be reached at (918) 749-5600 or joe@drjoemassad.com.
Disclosure: Dr. Massad was a member of the IRB research team to test the Eclipse system, and is an independent consultant for DENTSPLY Trubyte.
Dr. Lobel is assistant clinical professor at Tufts University School of Dental Medicine. He can be reached at lobeldmd@aol.com.
Dr. Garcia is professor and chair, Department of Prosthodontics, University of Texas Health Science Center, San Antonio. She is a diplomat of the American Board of Prosthodontics and fellow of the American College of Prosthodontists (ACP). She is secretary and chair of the Council for the American Board of Prosthodontics for ACP. Dr. Garcia co-authored the text Osseointegration and Occlusal Rehabilitation. She was named the 2004 ACP Educator of the Year, received the 1999 University of Colorado President’s Excellence in Teaching Award, and was awarded the designation of Rocky Mountain Study Club Professor of the Year, which is awarded by the private practice community. She maintains a practice limited to prosthodontics. She can be reached at garcialt@uthscsa.edu.
To comment on this article, visit the discussion board at dentistrytoday.com.


