Oral health and general health should not be interpreted as separate entities.
Our mouths are full of bacteria, various types of plaque, and biofilms. Oral health is an integral part of general health and is essential to the overall health and well being of man and animals. When we have plaque in our mouth, it can play havoc with other parts of our bodies because of bacteria and the inflammation it can cause.
Recent progress in the classification and identification of oral microorganisms and the realization that certain microorganisms are normally found in the oral cavity have opened the way for a more realistic assessment of the importance of oral focal infection. It has become increasingly clear that the oral cavity can act as the site of origin for the dissemination of pathogenic organisms to distant body sites, especially immunocompromised hosts such as patients suffering from malignancies, diabetes, rheumatoid arthritis, or receiving corticosteroid and other immunosuppressive treatments. A number of epidemiological studies have suggested that oral infection, especially marginal and apical periodontitis, may be a risk factor for systemic diseases.1 Human endodontic and periodontal infections are associated with complex microfloras in which approximately 200 species (in apical periodontitis) and more than 500 species (in marginal periodontitis) have been encountered. These infections are predominantly anaerobic, with Gram-negative rods being the most common isolates.1 The anatomic proximity of these microfloras to the bloodstream can facilitate bacteremia and systemic spread of bacterial products, components, and immunocomplexes.
It is the early identification of oral disease that may contribute to early diagnosis and treatment for a number of systemic factors. There are many health factors that can play a key role in periodontal disease. Which came first, the gum problems or the systemic problems? If bacteria, plaque, and biofilms live inside your mouth, who is to say these don’t invade the bloodstream through the oral cavity?
CURRENT VIEW OF RISK FACTORS AND PERIODONTAL DISEASES
| Chart. Adjunctive Therapies and Intervention. |
 |
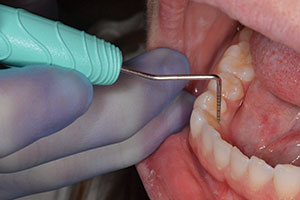
Periodontal infections are associated with specific pathogenic bacteria, which colonize in the subgingival area. At least 2 of these microorganisms, Porphyromonas gingivalis and Actinobacillus actinomycetemcomitans, also invade the periodontal tissue and are virulent organisms. Initially, the bacteria of periodontal disease and the progression of periodontal infections are clearly modified by local and systemic conditions called risk factors. The local factors include pre-existing disease as evidenced by deep probing depths and plaque retention areas associated with defective restorations.
Risk factors, which we know to be important, include diabetes mellitus, tobacco use, rheumatoid arthritis, peptic ulcers, respiratory disease/chronic obstructive pulmonary disease (COPD), cardiovascular disease, asthma, allergies, cancer, obesity, certain medications, and most recently also include Alzheimer’s disease.2 Recent studies also point to several other potentially important periodontal risk indicators. These include stress and coping behaviors as well as osteopenia associated with estrogen deficiency.3 Background determinants are also associated with periodontal disease, including gender (with males having more disease), age (with more disease seen in the elderly), and hereditary factors. Inflammation causes a host response to deal with the infection. When inflammation continues to be present, it can contribute to a number of systemic diseases/conditions. This article will discuss many of these (Chart).
DIABETES
Diabetes mellitus and periodontal disease are 2 very common chronic diseases in the United States, especially in individuals whose metabolic control is poor and who use tobacco. Diabetes and use of tobacco are 2 risk factors that affect the initiation and progression of periodontitis. Our attempts to manage these factors are now an important component of prevention and the treatment of adult periodontitis. Diabetes is an important link, because patients with this disease generally have increased susceptibilities to many types of infections, particularly Gram-negative anaerobic bacteria. High blood sugar levels help bacteria grow, which can lead to periodontal disease. Many studies have shown a positive relationship between poor glycemic control and increased incidences of periodontitis.4
Additionally, impaired neutrophil function has been demonstrated in diabetic patients. The future in medically treating these patients to manage diabetes needs to include a referral to the dental office for a dental/periodontal exam and possible treatment.
CARDIOVASCULAR DISEASE
The body contains 40 billion blood vessels, which makes it simple for harmful inflammatory byproducts to remain anywhere inside arteries, feeding the heart and brain.5 An underlying inflammatory response may place an individual at high risk for both periodontal disease and atherosclerosis. An inflammatory process probably has sources that may include systemic inflammation and local infections (eg, connective tissue diseases, gingivitis, prostatitis, bronchitis, urinary tract in-fections, gastric inflammation). Newer analyses have examined CRP (C-reactive pro-tein levels—a marker of inflammation) or cytokines.5 Cytokines have been used as a marker of inflammation and a higher incidence of heart attack.
PRETERM LOW-BIRTHWEIGHT BABIES
Gram-negative anaerobic bacterial infections that occur with periodontal disease are commonly observed in women of childbearing age. Newly devised techniques to measure matrix metalloproteinases (MMPs) levels in amniotic fluid allowed scientists to discover that certain MMP levels rise while others fall in association with premature rupture of membranes and with spontaneous labor. These observations strongly support the theory that MMPs play a critical role in events leading to premature labor. The findings support the notion that premature labor is the consequence of an immune response to infections of the uterus in some women and their infants. Scientists can now work to identify the genetic factors that predispose some women to premature labor, discover new ways of preventing the heightened immune response, and ultimately prevent premature labor.6 We know that MMPs play an important role in periodontal disease and the inflammatory response, therefore having a healthy mouth can lead to a healthy, full-term pregnancy.
MEDICATIONS AS A RISK FACTOR FOR PERIODONTITIS
Significant gingival enlargement (hyperplasia) has been noted with the following medications: phenytoin, calcium channel blockers (particularly nifedipine, verapamil, diltiazem, and oxodipine), and cyclosporin. Xero-stomia is a potential side effect of medications. Medications that cause xerostomia include antihypertensives, antihistamines, narcotic analgesics, quinalones, some tranquilizers, and tricyclic antidepressants. Many of the antianxiety/antidepressant drugs can cause xerostomia, which in return may not only cause decay, but can exacerbate gingivitis and periodontal disease. It is imperative to update a patient’s medical history each time he or she is seen as a patient in the dental office.
RHEUMATOID ARTHRITIS AND OSTEOPOROSIS
Rheumatiod arthritis (RA) is a disorder in which the body attacks its own healthy cells and tissues. Patients who are diagnosed with rheumatoid arthritis are found to have membranes surrounding the joints, which become inflamed and release enzymes that cause the surrounding cartilage and bone to wear away. In severe cases, other tissues and body organs can also be affected. Studies have found an increased risk of bone loss and fracture in individuals with rheumatoid arthritis.7 People with rheumatoid arthritis are at increased risk for osteoporosis for many reasons. To begin with, the glucocorticoid medications often prescribed for the treatment of RA can trigger significant bone loss. Tissue Necrosis Factor Alpha (TNFa) is an enzyme known to destroy osteoclasts and cause bone loss not only systemically, but also in the oral cavity. This enzyme is prevalent in RA patients.
RESPIRATORY DISEASES
Several microbiologic and epidemiologic studies have suggested an association between dental plaque, poor oral health, and respiratory diseases.8 A number of hypotheses are suggested to explain how oral bacteria may participate in the pathogenesis of respiratory infection. It is suggested that oral secretions are likely aspirated along with respiratory pathogens and may affect the adhesion of the organisms to the respiratory epithelium. In addition, oral bacterial products or cytokines in oral/pharyngeal aspirates may stimulate cytokine production from respiratory epithelial cells, resulting in recruitment of inflammatory cells. Other preliminary data are presented that some species of oral bacteria may induce the release of proinflammatory cytokines from epithelial cell lines to an extent similar to that seen for respiratory pathogens.8
PEPTIC ULCERS
Research has now shown that H. pylori strains having similar virulence markers are able to induce different types of gastric inflammation and injury. The entire genome microarray of H. pylori revealed distinctions in the ability of H. pylori strains to induce epithelial cell responses, which are related to inflammation.9
| Table 1. Therapeutic Strategies for the 21st Century. |
|
Reduction of Risk Factors: Reduce Bacterial Load: |
CANCER
Cytokines include many types of proteins, which can cause inflammation not only in the mouth but throughout various parts of the body. There are several members of the cytokine family (Chart). RANKL is a member of the TNF superfamily of cyto-kines. The protein was initially identified as a cytokine with an ability to stimulate T-cell and dendritic cell function. It was termed TRANCE–TNF-related activation-induced cytokine, or alternatively as RANKL. It has been cloned independently by 2 groups due to its ability to stimulate osteoclast differentiation, activity, and survival. In general, the TNF family of cytokines have the ability to cause bone loss systemically and orally.10
TOBACCO USE
This is one risk factor that is preventable. Tobacco use causes chronic systemic inflam-mation because of toxins found in the body and can stimulate platelets to clump together. The body will go into “high gear” to fight this, causing inflammation that can result in various medical conditions.
|
Table 2. Web Sites for Periodontal Disease and Research. |
| (1) cochrane.org—International Healthcare Information/Systematic Reviews (2) ncbi.nlm.nih.gov/entrez/query.fcgi—PubMed/National Institute of Health Library (3) forsyth.org—National Center for Evidence-Based Health (4) thejcdp.com—Journal of Contemporary Dental Practice |
CONCLUSION
Systemic health is closely linked to the state of the oral cavity. Evidence is mounting that the presence of inflammation in the blood may signal an increased risk for various diseases. For the future, it is important that we as dental healthcare providers incorporate diagnostic tests to identify patients who have the greatest risk for diseases other than dental disease. It is important that each dental visit begin with a thorough review of the patient’s medical history. For patients who have periodontal pockets of 5 mm or greater, it is the standard of care to recommend scaling and root planing. We are now able to treat these deep pockets with various, locally applied antimicrobials such as Arestin, Atridox, and PerioChip. For patients who are immunocompromised, use tobacco, or have chronic periodontitis, host modulation therapy shows strong evidence of increasing the patient’s response to nonsurgical periodontal treatment (Table 1).
Subantimicrobial doses of doxycycline (SDD or Periostat) can be used as an adjunct to definitive scaling and root planing. Strong evidence supports the use of SDD as an adjunct to conventional therapy in the management of chronic periodontitis.11 Referral to a primary care physician is indicated when a medical concern is found. Dentists, dental hygienists, dental auxiliaries, and other members of the dental team need to keep abreast of the latest research by attending conferences, reading their professional journals, and checking the medical/dental Web sites (Table 2).
Much research on the inflammatory process and its relationship to oral and systemic diseases is currently underway, and the information we receive will change constantly as research progresses on this important topic.
References
- X Li, Kolltveit KM, Tronstad L, et al. Systemic diseases caused by oral infection. Clin Microbiol Rev. 2000;13:547-558.
- Microbe linked to Alzheimer’s. CBSnews.com Web site. Available at: http://www.cbsnews.com/stories/1998/11/24/health/main23470.shtml. Accessed September 15, 2004.
- Wimmer G, Janda K, Wieselmann-Penkner K, et al. Coping with stress: its influence on periodontal disease. J Periodontol. 2002;73:1343-1351.
- Cutler CW, Machen RL, Jotwani R, et al. Heightened gingival inflammation and attachment loss in type 2 diabetics with hyperlipidemia. J Periodontol. 1999;70:1313-1321.
- P1 Periodontal Disease as a Risk for CVD, CHD, and Stroke. AHA journals Web site. Available at: http://www.ahajournals.org/cgi/search?journalcode=all&fulltext=Markers+of+Inflammationa+and+Cardiovascular+Disease&x=5&y=7. Accessed September 14, 2004.
- Maymon E, Romero R, Pacora P, et al. Evidence of in vivo differential bioavailability of the active forms of matrix metalloproteinases 9 and 2 in parturition, spontaneous rupture of membranes, and intra-amniotic infection. Am J Obstet Gynecol. 2000;183:887-894.
- Scannapieco FA, Ho AW. Potential associations between chronic respiratory disease and periodontal disease: analysis of National Health and Nutrition Examination Survey III. J Periodontol. 2001;72:50-56.
- Mercado FB, Marshall RI, Bartold PM. Inter-relationships between rheumatoid arthritis and periodontal disease. A review. J Clin Periodontol. 2003;30:761-772.
- Gebara EC, Pannuti C, Faria CM, et al. Prevalence of Helicobacter pylori detected by polymerase chain reaction in the oral cavity of periodontitis patients. Oral Microbiol Immunol. 2004;19:277-280.
- Lam J, Nelson CA, Ross FP, et al. Crystal structure of the TRANCE/RANKL cytokine reveals determinants of receptor-ligand specificity. J Clin Invest. 2001;108:971-979.
- Reddy MS, Geurs NC, Gunsolley JC. Periodontal host modulation with antiproteinase, anti-inflammatory, and bone-sparing agents. A systematic review. Ann Periodontol. 2003;8:12-37.
Ms. Seidel-Bittke is founder of Dental Practice Solutions, an evolutionary dental consulting business specializing in a team approach to treating periodontal disease while raising the value of patient services. She graduated from the University of Southern California with a bachelor’s degree in dental hygiene in 1984. She is a former clinical assistant professor at USC and most recently has been a guest lecturer for the Contemporary Practice Management course at USC. She can be reached for comments or to schedule speaking for dental conferences at (866) 206-6364 or debra@dentalpracticesolutions.com, or visit dentalpracticesolutions.com.