The use of herbal supplements by the American public as nonprescription therapeutic or preventive products has increased steadily in the last 2 decades. For instance, Eisenberg and colleagues1 reported that from 1990 to 1997, utilization of self-prescribed herbal medications among adult Americans increased from 2.2% to 12%, and the percentage of individuals consulting herbal medicine practitioners rose from 10.2% to 15.1%. A more recent survey conducted by Prevention Magazine2 demonstrated that as much as 33% of American adults used herbal supplements in 2000. Even greater use of these products has been reported among elderly and medically compromised patients.3,4 However, many of the consumers are unaware of the potential adverse effects of these substances, and about 70% of them do not reveal the use of herbal supplements to their healthcare providers.1,3-5
Being categorized as dietary supplements by the Dietary and Supplement Health and Education Act of 1994, herbal products are not regulated by the FDA with the same scrutiny as conventional drugs.1,6-8 This has raised concerns about their safety and efficacy, with the possibility of causing health risks. Health problems associated with herbal supplements have been reported in the media, by poison control centers, by government agencies, and in scientific journals. These problems arise from the improper use of these products, the actual product contents, product tampering, and product defects that can change product identity, quality, purity, strength, and/or composition.5,7,8
In view of the reported biological effects and the potential toxicity of herbal supplements, it is imperative that health professionals be knowledgeable about precautions regarding these natural products. Since dental patients are likely to use herbal supplements for various health/nutritional reasons, dentists and dental hygienists need to be able to take appropriate measures in the event of possible problems that may arise as a result of this. In this article, popular herbal supplements, that are likely to require modifications in managing a patient’s dental treatment when they are used, are briefly reviewed.
HERBAL SUPPLEMENTS WITH SYSTEMIC EFFECTS
Among the different types of herbal supplements commonly used by consumers, products with blood-thinning, hypotensive, and central nervous system (CNS) depressing properties, appear to have greater potential to require modifications when performing dental treatment. These products along with their frequently reported uses and the most relevant chemical constituents responsible for their pharmacological effects are listed in the table included in this article (See Table).
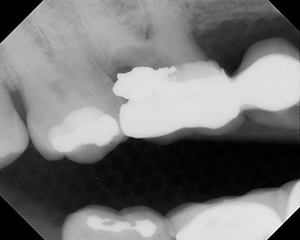
There are 2 categories of blood-thinning herbal supplements: antiplatelets and anticoagulants. While all the herbs listed under this category have the potential to enhance the risk of bleeding, the antiplatelets (garlic, ginger, and ginkgo) have been shown to exert a more serious effect in this regard.3,8-13 Blood-thinning herbal products can pose significant bleeding problems in dentistry after major oral and maxillofacial surgery. Bleeding can also be a nuisance during the performance of minor surgical procedures.14 Because of this, most hospitals are increasingly requiring surgical patients to quit taking specific herbal supplements for up to 2 weeks prior to surgery.15,16 A second consideration is the possibility of postoperative bleeding if practitioners prescribe nonopioid analgesics (such as aspirin) and nonsteroidal anti-inflammatory drugs (such as ibuprofen) for postoperative pain relief.7-13 This potential herb-drug interaction may be avoided if drugs such as acetaminophen (Tylenol [McNeil]), opioids, and the cyclooxygenase-2 selective analgesics like rofecoxib (Vioxx [Merck]) are prescribed.
Also shown in the Table are the cardiovascular-inhibiting hypotensive herbals astralagus, dong quai, and sag. By lowering arterial blood pressure, these herbs may induce orthostatic hypotension in patients who take them in sufficient doses.7,17 This problem is more likely to occur in the elderly, in those with cardiovascular disorders, and in patients fasting for sedation or anesthesia procedures.3,7 It is important that such patients should be closely monitored for hypotension. Furthermore, changes in body position (ie, from supine to standing position) should be made slowly and with careful observation of the patients.7
Several herbal supplements are known to cause CNS depression, especially kava and valerian, which are also listed in the Table.3,7,10-13,15,17,18 These herbs induce CNS depression primarily by activating the gamma-aminobutyric acid neurotransmission and receptor function. The combination of these herbal products with CNS depressing conventional drugs, such as standard doses of anxiolytics (eg, diazepam), and sedative-hypnotics (eg, chloral hydrate) may yield further CNS depression. On the other hand, long-term use of these herbal products may reduce responsiveness to benzodiazepines (eg, diazepam) and related drugs.7,11-13,18
 |
HERBAL SUPPLEMENTS WITH VARIOUS PHARMACOLOGICAL EFFECTS
Among other herbal supplements popularly used by consumers, St. John’s wort and ephedra (Mahuang) are more relevant to be discussed in relation to their effects on dental treatment.
St. John’s wort is commonly used as an antidepressant for mild to moderate depression, and sometimes it is also taken for problems of anxiety, insomnia, and inflammation.7,11-13,17,19 Some of its constituents (primarily hypericin and hyperforin) have been shown to inhibit monoamine oxidase and block neuronal reuptake of endogenous amines in the CNS as well as in the periphery. It is recommended that the opioid analgesics, meperidine and tramadol (with unique properties), be avoided in patients taking St. John’s wort. This is because of the possibility of increased serotonin activity in the brain that may result in a serotonergic syndrome of restlessness, motor hyperactivity, and coma, among other effects.11,13,18,19 St. John’s wort may also interact with many other drugs due to its ability to stimulate CYP-450 enzymes and P-glycoprotein transporter, in addition to other effects.7,12,13,19 Consequently, increased metabolism and excretion of many drugs can occur in the presence of this popular herbal supplement. Of dental significance, in this regard, is the enhancement of first-pass metabolism and thus reduced effectiveness of triazolam and related benzodiazepines observed in the presence of St. John’s wort.7,12,13,19 A few incidences of orthostatic hypotension have also been reported in patients taking St. John’s wort.7,12,19
Ephedra (Mahuang) is popularly used for weight reduction, energy enhancement, and asthma treatment.3,8,11-13,17,18 It produces increased sympathomimetic activity, due to the presence of sympathomimetic alkaloid constituents such as ephedrine, pseudoephedrine, and norephedrine. The biological effects of these substances include stimulation of both the CNS and the cardiovascular system.3,8,11,12 Because of this, ephedra (in relatively high doses) induces significant adverse neurological and cardiac effects of varying kinds including: insomnia, hyperactivity, nervousness, and tachycardia/arrhythmias. These conditions, among other possible adverse effects, result in reduced effectiveness of anxiolytics, sedative-hypnotics, general anesthetics, and other related CNS-acting drugs. Ephedra is also implicated in arrhythmias when used with halothane.3,11,12 Under these situations, there may be a need to stop taking the herb or adjust the doses of the CNS depressing conventional drugs.
MODIFICATIONS FOR PATIENTS ON HERBAL SUPPLEMENTS
The documentation that herbal supplements are commonly used by the American public suggests that health professionals be knowledgeable about precautions regarding these products. An understanding of the pharmacology of herbs would then allow clinicians to make appropriate treatment modifications depending upon the type and doses of herbal supplements used by dental patients.
Modifications may involve stopping herbal supplements prior to dental procedures/treatment, or adjusting the dental procedures/treatment plans. Realizing the medical problems associated with the use of some herbs, the American Society of Anesthesiologists and the American Academy of Orthopedic Surgeons recommend that patients should discontinue herbal medications at least 2 weeks prior to surgery. Accordingly, as noted above, most hospitals are increasingly requiring patients to quit taking specific herbal supplements for up to 2 weeks before surgery. It is expected that patients undergoing similar procedures in dental clinics will benefit if the same requirement is demanded from them, in addition to taking appropriate actions to avoid other risks that can be caused by herb-drug interactions and/or patients’ health conditions. To achieve this goal, dental practitioners and hygienists should first obtain information from patients on the use of herbal supplements and educate themselves about the products reported using available reliable sources of scientific information.
References
- Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280:1569-1575.
- Johnston BA. Prevention Magazine assesses use of dietary supplements. HerbalGram. 2000;48:65.
- Ciocon JO, Ciocon DG, Galindo DJ. Dietary supplements in primary care. Botanicals can affect surgical outcomes and follow-up. Geriatrics. 2004;58:20-24.
- Tsen LC, Segal S, Pothier M, et al. Alternative medicine use in presurgical patients [published correction appears in Anesthesiology. Nov 2000;93:1371]. Anesthesiology. Jul 2000;93:148-151.
- Bent S, Ko R. Commonly used herbal medicines in the United States: a review. Am J Med. 2004;116:478-485.
- US Food and Drug Administration, Center for Food Safety and Applied Nutrition. Dietary supplement health and education act of 1994. http://vm.cfsan.fda.gov/~dms/dietsuppl.html. Published December 1, 1995. Accessed November 15, 2008.
- Yagiela JA, Dowd FJ, Neidle EA. Pharmacology and Therapeutics for Dentistry. 5th ed. St Louis, MO: Mosby; 2004:185-186.
- Abebe W. An overview of herbal supplement utilization with particular emphasis on possible interactions with dental drugs and oral manifestations. J Dent Hyg. 2003;77:37-46.
- Abebe W. Herbal supplements having the potential to interfere with blood clotting. GDA Action. 2003;22:23-26.
- Abebe W. Herbal medication: potential for adverse interactions with analgesic drugs. J Clin Pharm Ther. 2002;27:391-401.
- Abebe W. Herbal supplements. Any relevancy to dental practice? N Y State Dent J. 2002;68:26-30.
- Ang-Lee KM, Moss J, Yuan CS. Herbal medicines and perioperative care. JAMA. 2001;286:208-216.
- Ernst E. The risk-benefit profile of commonly used herbal therapies: Ginkgo, St. John’s Wort, Ginseng, Echinacea, Saw Palmetto, and Kava [published correction appears in Ann Intern Med. Jan 2003;136:42-53]. Ann Intern Med. Jan 2002;136:42-53.
- American Academy of Orthopedic Surgeons. Herbal supplements and their interactions with medication. http://orthoinfo.aaos.org/topic.cfm?topic=A00206. Updated July 2007. Accessed November 21, 2008.
- Leak JA. Potential hazards of perioperative herb and supplement use. ASA Refresher Courses in Anesthesiology. 2003;31:117-126.
- Norred CL, Zamudio S, Palmer SK. Use of complementary and alternative medicines by surgical patients. AANA J. 2000;68:13-18.
- Gruenwald J, Brendler T, Jaenicke C, et al (eds). PDR for Herbal Medicines. Montvale, NJ: Medical Economics Co; 1999:719-728.
- Jacobsen PL, Cohan RP. Alternative dental products. J Calif Dent Assoc. 1998;26:191-198.
- Abebe W. St. John’s wort: potential interactions with dental drugs. GDA Action. 2005;25:18-20.
Dr. Abebe graduated from the University of British Columbia, Vancouver, Canada, in 1990, with a PhD in pharmacology. Currently, he is an assistant professor in the Department of Oral Biology at the Medical College of Georgia School of Dentistry in Augusta, Ga. He teaches pharmacology to dental students and residents. In addition to conducting research on the use and effects of herbal supplements, he has studied the vascular effects of dental materials and diabetes mellitus. He is the author and co-author of more than 48 scientific articles, which have been published in peer-reviewed journals. He is a member of several professional associations related to pharmacology and dentistry. He can be reached at wabebe@mail.mcg.edu.
Dr. Smith did not report any disclosures.