Part 1 of this series discussed cardiovascular disease, cardiac emergencies, and the rationale behind the concept of early defibrillation in response to a cardiac emergency. Part 2 will discuss the use of new Automated External Defibrillators (AEDs) and their potential importance in dental practice.
THE AUTOMATED EXTERNAL DEFIBRILLATOR
AEDs are sophisticated, battery-operated (the batteries in AEDs last up to 5 years, according to the manufacturers), computerized devices that have been shown to be reliable and easy to operate. Their availability, prior to the arrival of EMS, enables lay rescuers with minimal training to administer the critically important step of defibrillation. AEDs are employed by flight attendants,1 security personnel,2 family members,3 and school-age children4. They are found in airports, airplanes, casinos, high-rise office buildings, shopping malls, recreational facilities and are used by healthcare professionals5 in ambulances, hospitals, physicians’ offices, and dental clinics.6-8
AEDs are actually semiautomated, because the AED advises the operator that a shock is (or is not) indicated, but will not deliver the shock without the rescuer activating the unit (eg, pushing the shock button). The AED records and analyzes the ECG signal to determine if it is consistent VF (ventricular fibrillation) or pulseless VT (ventricular tachycardia), 2 conditions associated with cardiac arrest (Figures 1 and 2).9 The AED then advises a shock when an ECG signal consistent with these rhythms is detected. These devices are extremely accurate in their ability to analyze cardiac rhythms.10
| Table 1. |
| Use AED only when all of the following are present:13
•Unresponsiveness * Signs of circulation, for the healthcare provider, include pulse, signs of normal breathing, |
AEDs should be employed only when cardiac arrest has been confirmed and only when all movement has ceased11 (see Table 1). Failure to follow manufacturer’s instructions for use has—on rare occasions (<0.1%)—resulted in the delivery of an inappropriate shock.12
Before applying the AED electrodes, the rescuer must determine if any special situations exist that require modification of—or contraindicate the use of—the AED. Such situations include the following: (1) victim is <8 years of age or <25 kg (55 lb, athough recently introduced AEDs may be used in children); (2) victim is in or near standing water (eg, edge of swimming pool); (3) victim has an implanted pacemaker or ICD (implanted cardioverter/defibrillator); and (4) victim is wearing a transdermal medication patch of any type on skin where the AED electrode is to be placed. The patch should be removed and the area thoroughly dried.13
| Table 2. |
| Use of the AED (automated external defibrillator)
•Store AED beside a telephone. |
Although numerous manufacturers market AEDs in the United States, most operate in the same way and have similar components. The American Heart Association (AHA) recommends that AEDs be stored beside a telephone, permitting the rescuer to activate EMS rapidly and deliver the AED to the scene of the cardiac arrest promptly. Once available, the AED should be placed close to the victim’s left ear. Table 2 presents the 4 universal steps in AED operation.
Once the power is turned on (step 1), the AED’s voice prompt directs the rescuer to attach electrodes to the patient (step 2). Each adhesive pad has a diagram of the chest indicating its proper placement location (Figure 3). One electrode is placed on the upper-right sternal border directly below the clavicle; the other lateral to the left nipple, with the top margin of the pad a few inches below the axilla (Figure 4). If wet, the chest should quickly be dried. If the chest is excessively hairy, the pad may not achieve contact with the skin. The AED will indicate this by repeating “check electrodes” or “attach electrodes.” Applying firm pressure may correct this problem. If not, quickly remove the electrode (taking hair with it) and reapply a new electrode. Once properly attached, the AED prompt will state “analyzing rhythm, do not touch patient” (step 3). No one should be touching the patient as any movement might influence the rhythm analysis by the AED. Rhythm analysis takes between 5 and 15 seconds (depending upon AED brand and rhythm present). If VT or VF is detected, the AED will prompt “shock advised,” then “charging,” and finally “charged.” The next prompts will be “stand back” and “press shock button.” Before pressing the shock button, it is important to clear all persons from contact with the victim. The lead rescuer should look and say, “I’m clear, you’re clear, everybody’s clear.” Delivery of the shock should only occur after all responders are clear of the victim.14 The shock button is pressed and a sudden contraction of the victim’s musculature will be noted (step 4).
After delivery of the first shock, CPR is not restarted. It is important to deliver the second and third shocks (if needed) as promptly as possible. The AED will automatically re-analyze the rhythm, and if VF/VT is still present, the AED will announce it (“shock indicated”) and it will go through the same sequence for a second and (if needed) third shock. Following delivery of a third shock, the AED immediately prompts the rescuer to “check airway, check breathing, check pulse. If no pulse, continue CPR.”
POTENTIAL OUTCOMES AFTER DEFIBRILLATION
There are 3 potential outcomes of defibrillation: (1) VT or VF is still present; (2) VT or VF is no longer present, but there is no palpable pulse; and (3) VT or VF is no longer present and a palpable pulse is present. The following text examines these 3 outcomes individually.
(1) “Shock indicated.” VF or VT is still present. Following 3 shocks, the AED prompts the rescuer to resume CPR for 1 minute, after which the AED prompts a check for breathing and pulse and an analysis of the rhythm. If VF or VT persists, the AED will deliver additional sets of 3 shocks alternating with 60 seconds of CPR until the AED gives a “no shock indicated” message or until ACLS (advanced cardiovascular life support) becomes available.15
(2) “No shock indicated; check airway, check breathing, check pulse. If
no pulse, continue CPR.” No pulse is detected. If, after delivery of any shock, the AED detects a rhythm that is neither VF nor VT, it will state that no shock is indicated. Following the delivery of 3 sets of shocks, there is a low probability that the detected rhythm can be corrected
(eg, asystole has probably occurred). CPR is resumed, but the prognosis for these victims is poor. In this situation, rhythm analysis should only be performed every 1 to 2 minutes.
(3) “No shock indicated; check airway, check breathing, check pulse. If no pulse continue CPR.” Pulse is detected. When a palpable pulse is present, but the unconscious adult victim is still apneic, rescue breathing at a rate of 1 ventilation every 5 seconds (12 per minute) is provided. If the victim is breathing adequately, place him on his side (recovery position), keeping the AED attached until the arrival of EMS personnel. Should VF or VT recur (which happens frequently) the AED will prompt the rescuer to check for signs of circulation, then proceed through the sequence described above.
TYPES OF AED
The concept underlying defibrillation is that the unit should deliver the lowest effective energy needed to terminate VF. If the energy and current are too low, VF will not be terminated; if it is too high, myocardial damage may result.
AEDs use 1 of 2 waveforms: monophasic or biphasic. Monophasic AEDs deliver current in one direction (from one electrode pad to the other). Biphasic waveforms deliver current that flows in a positive direction for a specified duration, then reverses to the negative or opposite direction in the second phase. As compared to biphasic units, more energy must be delivered with monophasic units. For monophasic AEDs, the recommended first-shock energy is 200 J (joules), second shock is 200 or 300 J, and the third shock is 360 J.16 The goal of escalating the energy dosage is to maximize success at terminating VF while minimizing myocardial damage.17 The higher shock energies (300 J and 360 J) are delivered only if the lower doses (200 J and 300 J) fail to convert the dysrhythmia. The AED automatically provides the appropriate dosage. Biphasic AEDs have been available in the USA since 1996, delivering nonescalating shocks of 150 J. Most currently introduced and available AEDs deliver biphasic waveform shocks.18
AEDS IN THE DENTAL OFFICE
Basic life support (BLS) certification is a requirement for dental licensure in many states. BLS for healthcare providers, as now defined, includes defibrillation.19 Nevertheless, no state dental board has mandated the availability of AEDs in the dental office (except where the doctor is permitted to administer parenteral conscious sedation or general anesthesia).
AEDs are easy to use, safe, have been proven to save lives, and are relatively inexpensive. (Some models are presently under $1,500.) In addition, AEDs are portable and can be taken home. (Approximately 70% to 80% of cardiac arrests occur in the home.)
In November 2002, the United States Food and Drug Administration approved the sale of AEDs to laypersons who live in home environments in which the likelihood of cardiac arrest is high.20 A prescription from a medical doctor is required before a layperson can obtain an AED, which can be purchased at some pharmacies.21,22
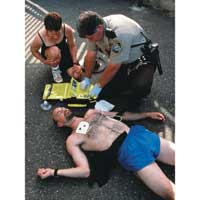
A CASE SCENARIO
In your office or in your home, a member of your office staff or a family member collapses. Trained in BLS, you quickly come to the victim’s side, shake the victim and yell at him, determining that he is unconscious. You yell to someone to call 9-1-1 as you start assessing the airway (head tilt-chin lift) and breathing (look, listen, feel). Noting no spontaneous respiratory efforts, you start rescue breathing—2 full, complete ventilations, seeing the victim’s chest rise each time. You next check for the carotid pulse for 10 seconds, but it is absent. Chest compression is started at a compression/ventilation ratio of 15 to 2. You yell to the person on the phone that the victim is in cardiac arrest.
| Table 3. |
|
Information to be given to EMS (9-1-1) operator23 1. The location of the emergency (with names of cross streets or roads or office or room number, if possible). To ensure that EMS personnel have no more questions, the caller should hang up only when instructed to do so by the EMS system operator |
When 9-1-1 is called, the primary EMS operator answers the phone within 5 to 10 seconds. You state that you have a medical emergency, then you are transferred to an EMS medical emergency operator (another 5 to 10 seconds passes). Table 3 lists the information that the caller should make available to the EMS operator.23
You are informed that the ambulance has been dispatched. Approximately 1 minute has elapsed. The ambulance requires a variable length of time to arrive, depending on your location and local response time.
Once the ambulance arrives at the scene, the EMS personnel gather their equipment and walk into the office or house, assessing the situation. They arrive at the victim’s side and prepare the AED for use. From ambulance arrival to initiation of defibrillation is probably an additional 2 minutes.
In the preceding scenario, in all likelihood the elapsed time from the moment of collapse to the delivery of the first shock is in excess of 10 minutes. Even with the delivery of ideal BLS, the expected survival rate in this scenario is 10% or less (at 9 to 11 minutes), and between 2% and 5% (beyond 12 minutes).24,25 These percentages could be markedly improved if the first shock was delivered after a shorter time interval following collapse. Wouldn’t you like to have a greater chance at survival if you were the victim?
| Table 4. | ||||||||||||||||||||||||||||||||
|
Table 4 lists many of the manufacturers of AEDs in the United States. Online sites offering different AEDs include aedsuperstore.com and medekit.com.
 |
| Figure 1. Ventricular tachycardia (VT). |
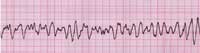 |
| Figure 2. Ventricular fibrillation (VF). |
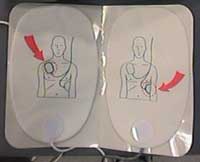 |
| Figure 3. AED electrodes (adult). |
 |
| Figure 4.Placement of AED pads (courtesy of Cardiac Science, Inc). |
CONCLUSION
The most frequent initial rhythm in witnessed sudden cardiac arrest is ventricular fibrillation, and the most effective treatment for VF is electrical defibrillation. The probability of successful defibrillation diminishes rapidly over time; therefore, reducing the elapsed time between cardiac arrest and defibrillation is critical for successful resuscitation. The use of new automated external defibrillators in cases of out-of-hospital cardiac arrest can significantly decrease the time between collapse and defibrillation.
References
1. Wolbrink A, Borrillo D. Airline use of automatic external defibrillators: shocking developments [see comments]. Aviat Space Environ Med 1999;19:179-186.
2. Valenzuela TD, Roe DJ, Nichol G, et al. The Casino Project: implications for public access defibrillation. Academic Emerg Med. 2000;7:426.
3. Eisenbe
rg MS, Moore J, Cummins RO, et al. Use of the automatic external defibrillator in homes of survivors of out-of-hospital ventricular fibrillation. Am J Cardiol. 1989;63:443-446.
4. Gundry JW, Comess KA, DeRook FA, et al. Comparison of naïve sixth-grade children with trained professionals in the use of an automated external defibrillator. Circulation. 1999;100:1703-1707.
5. Weisfeldt ML, Kerber RE, McGoldrick RP, et al. Public access defibrillation: a statement for healthcare professionals from the American Heart Association Task Force on Automatic External Defibrillation. Circulation. 1995;92:2763.
6. O’Rourke MF, Donaldson E, Geddes JS. An airline cardiac arrest program [see comments]. Circulation. 1997;96:2849-2853.
7. Valenzuela TD, Roe DJ, Nichol G, et al. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343:1206-1209.
8. Kaye W, Mancini ME. Improving outcome from cardiac arrest in the hospital with a reorganized and strengthened chain of survival: an American view [editorial]. Resuscitation. 1996;31:181-186.
9. Stults KR, Cummins RO. Fully automatic vs shock advisory defibrillators: what are the issues? J Emerg Med Serv. 1987;12:71-73.
10. Cummins RO, Eisenberg M, Bergner L, et al. Sensitivity, accuracy, and safety of an automatic external defibrillator. Lancet. 1984;2:318-320.
11. Dickey W, Dalzell GW, Anderson JM, et al. The accuracy of decision-making of a semi-automatic defibrillator during cardiac arrest. Eur Heart J. 1992;13:608-615.
12. Sedgwick ML, Watson J, Dalziel K, et al. Efficacy of out of hospital defibrillation by ambulance technicians using automated external defibrillators. The Heartstart Scotland Project. Resuscitation. 1992;24:73-87.
13. American Heart Association. BLS for Healthcare Providers. Dallas, Tex: American Heart Association; 2001:95.
14. Gibbs W, Eisenberg M, Damon SK. Dangers of defibrillation: injuries to emergency personnel during patient resuscitation. Am J Emerg Med. 1990;8:101-104.
15. American Heart Association. BLS for Healthcare Providers. Dallas, Tex: American Heart Association; 2001:101.
16. Weaver WD, Cobb LA, Copass MK, et al. Ventricular defibrillation – a comparative trial using 175-J and 320-J shocks. N Engl J Med. 1982;307:1101-1106.
17. Kerber RE, Martins JB, Kienzle MG, et al. Energy, current, and success in defibrillation and cardioversion: clinical studies using an automated impedance-based method of energy adjustment. Circulation. 1988;77:1038-1046.
18. Bardy GH, Gliner BE, Kudenchuk PJ, et al. Truncated biphasic pulses for transthoracic defibrillation. Circulation. 1995;91:1768-1774.
19. Cummins RO, Hazinski MF, Kerber RE, et al. Low-energy biphasic waveform defibrillation: evidence-based review applied to emergency cardiovascular care guidelines: a statement for healthcare professionals from the American Heart Association Committee on Emergency Cardiovascular Care and the Subcommittees on Basic Life Support, Advanced Cardiac Life Support, and Pediatric Resuscitation. Circulation. 1998;97:1654-1667.
20. The American Heart Association in collaboration with the International Liaison Committee on Resuscitation. Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care: part 4: the automated external defibrillator: key link in the chain of survival. Circulation. 2000;102(suppl I)I-60–I-76.
21. Anonymous. A shock at home can save a life. For some people it makes sense to have an automated external defibrillator. Harv Heart Lett. 2003;13(5):6-7.
22. Anonymous, Home Defibrillation, from http://www.cvs.com.
23. Chandra NC, Hazinski MF, Stapleton E. Instructor’s Manual for Basic Life Support. Dallas, Tex: American Heart Association; 2000.
24. McIntyre KM. Cardiopulmonary resuscitation and the ultimate coronary care unit [editorial]. JAMA. 1980;244:510-511.
25. Larson MP, Eisenberg MS, Cummins RO, et al. Predicting survival from out-of-hospital cardiac arrest: a graphic model. Ann Emerg Med. 1993;22:1652-1658.
Dr. Malamed is a professor of anesthesia and medicine at the School of Dentistry at the University of Southern California.