Often when a permanent molar erupts, the occlusal caries process develops before the tooth is fully erupted into the mouth. This leaves the practitioner with the dilemma of either attempting to seal a tooth with a traditional resin sealant in an extremely difficult area or waiting until the tooth is erupted to evaluate further. Erupting teeth can be exposed to prolonged acid attack under the operculum with no chance of re-mineralization occurring for many months.1
Practitioners often encounter a frank carious lesion needing restoration if the “wait-and-see” philosophy is used. Unsealed occlusal surfaces with early enamel lesions have a 4 times higher chance of developing dentinal lesions, according to one study.2 Also, according to Washington Dental Service, children who develop cavities on their molars will require an average of $2,187 to maintain each filling over their lifetimes.3
Clearly, preventing caries on erupting molars can have a profound public health benefit. Glass ionomer sealants have several potential advantages over resin sealants, including their ability to bond to tooth structure without the etching, rinsing, and bonding steps, and their ability to be used in areas of minimal isolation. Glass ionomer cement (GIC) is the only hydrophilic restorative material available;4 it leaches fluoride, strengthening enamel against future acid attacks, and may be bactericidal. Glass ionomer also reduces demineralization and at the same time increases remineralization.5 GIC sealants can serve as fluoride reservoirs in the oral cavity and contribute to retaining a low fluor-ide level in oral fluids, thereby contributing to the remineralization process of other teeth as well decreasing the incidence of dental caries.
The case described below uses Fuji GC Triage (GC America), which has a salmon pink shade that improves visibility during application and enables future inspection for retention evaluation. Another feature of Triage is its “command set” property, which can reduce set time by 30%. It also has a fluor-ide release level that is reportedly 6 times that of any other glass ionomer.6 The self-mix application of this glass ionomer cement sealant not only helps prevent caries on the partially erupted molar, but strengthens the enamel surface, making any future treatment of the tooth potentially more successful.
CASE REPORT
 |
 |
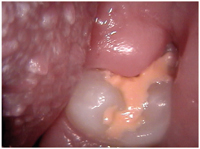
| Figures 1a and 1b. Preoperative photographs showing partially erupted lower second molars with operculum covering the occlusal surfaces. |
An 11-year-old female patient presented for a routine examination. Radiographs were unremarkable other than showing normally developing second molars not quite into the plane of occlusion. Clinical examination revealed partially erupted second molars Nos. 18 and 31 with significant amounts of plaque in an otherwise relatively clean mouth (Figures 1a and 1b). These teeth had relatively deep occlusal grooves retaining notable amounts of plaque. No carious lesions were detected with visual examination done with 3.5x power loupes; bite-wing radiographs were not indicated due to the patient’s orthodontic brackets. A review of prior bite-wings and a panoramic radiograph was negative for interproximal caries. Periodontal evaluation was within normal limits, and medical history revealed no significant findings.
This patient had no prior incidence of carious lesions in permanent teeth, however, several fillings had been placed in her primary teeth. Resin sealants were noted on teeth Nos. 3, 14, 19, and 30. The patient also had full-mouth orthodontic appliances. A caries risk assessment placed this patient into the moderate range. The teeth were cleaned with a DENTSPLY Prophy-Jet with sodium bicarbonate and water slurry to remove as much plaque as possible prior to DIAGNOdent (KaVo) evaluation. DIAGNOdent readings on teeth Nos. 18 and 31 were 17 and 15, respectively.
Alternative treatments were explained to both the patient and parent. These included waiting and watching, or placement of a glass ionomer sealant to remineralize and strengthen the newly erupting molar. Both the parent and patient opted for GIC sealants despite the fact that the average longevity for the sealant to stay in place would be less than 2 years. Ideally, a resin sealant could then be placed on each of these teeth. They also understood that placement of the sealants would contribute to a stronger occlusal surface.
TREATMENT PROCESS
 |
 |
| Figures 2. Prophy-Jet polish of occlusal surface. Care must be taken to avoid gingival bleeding. | Figures 3. Manipulation of Triage on occlusal surface with microbrush. |
 |
 |
| Figures 4. Immediate postoperative view. | 5a. |
 |
| Figures 5a and 5b. Similar case at 12 months. While a portion of the glass ionomer sealant has been lost on tooth No. 18, the DIAGNOdent reading is only 7. |
Each side of the mouth was isolated with the Isolite (Isolite Systems), and each lower second molar was treated individually. The teeth were cleaned with a DENTSPLY Prophy-Jet with sodium bicarbonate and water slurry to remove plaque, being careful not to disturb the gingival tissue adjacent to the occlusal surface in order to minimize bleeding (Figure 2). The teeth were then dried with a stream of air, and a capsule of GC Fuji Triage was activated, triturated for 20 seconds, and placed on the occlusal surface of the tooth. This increment of Triage was carefully teased under the gingival operculum and on the exposed occlusal surface with a microbrush (Denbur; Figure 3). Following placement, a halogen curing light (Kerr/Demetron) was used in close proximity to the sealant for 20 to 40 seconds to initiate the “command set” from the heat of the light. After 105 seconds of setting time, the material was hard enough to evaluate and adjust occlusion (Figures 4 to 5b).
DISCUSSION
Although it is generally acknowledged that a resin sealant is retained longer than a glass ionomer sealant, the end result is similar.2 This can be attributed to the enamel’s fluoride uptake while in contact with the GIC and the potential of a small amount of GIC to remain in the deep fissure of the tooth. In an erupting molar, it is not possible to resin bond successfully to aprismatic, hypocalcific, or demineralized enamel.1 Thus, patients needing sealant protection for caries prevention are the least likely to have long-term retention of traditional resin sealants. Despite the inevitable loss of the GIC sealant, the enamel surface will subsequently be stronger and more caries resistant, regardless of future treatment.2 Therefore, sealing newly erupted permanent molars with high-filled glass ionomer may be a caries-preventive measure especially appropriate for high-risk children.
References
1. Milicich G. The dawn of a new era. Presented at: World Congress of Minimally Invasive Dentistry. August 2004; San Francisco, Calif.
2. Taifour D, Freneken JE, van’t Hof MA, et al. Effects of glass ionomer sealants in newly erupted first molars after 5 years: a pilot study. Community Dent Oral Epidemiol. 2003;31:314-319.
3. Dental money pit: the $2000 Cavity. Check Up (A Quarterly Newsletter). Boston, Mass: Delta Dental Dental Plan of Massachusetts Publication; Spring 2005:3.
4. McLean JW. Clinical applications of glass-ionomer cements. Oper Dent. 1992;5(suppl):184-190.
5. Chadwick BL, Treasure ET, Playle RA. A randomised controlled trial to determine the effectiveness of glass ionomer sealants in pre-school children. Caries Res. 2005;39:34-40.
6. Herle GP, Joseph T, Varma B, et al. Comparative evaluation of glass ionomer and resin based fissure sealant using noninvasive and invasive techniques: a SEM and microleakage study. J Indian Soc Pedod Prev Dent. 2004;22:56-62.
Dr. Evans is a fellow in the AGD, the World Congress of Minimally Invasive Dentistry, and The World Clinical Laser Institute. He maintains a private practice of 25 years in Chewelah, Wash. He can be reached at (509) 935-8642 or drbud@chewelahdentistry.com.
To comment on this article, visit the discussion board at dentistrytoday.com.











