
A disinfection system at BJC HealthCare in St. Louis that uses vaporized hydrogen peroxide allows personnel to reuse their own N95 respirator masks up to 20 times and ensures that they are the only people who ever touch their mask.
“Our primary outcome is safety for the healthcare worker,” said project leader and study coauthor Andrew Pierce, MHSA, director of supply plus at Barnes-Jewish Hospital. “We want to make it safer for team members who are at risk while taking care of patients with a known or possible COVID-19 diagnosis.
Developed in collaboration with the Washington University School of Medicine, the program uses a procedure first tested by Duke University in 2016. However, the Barnes-Jewish process also uses an identification system that enables the hospital to return the sanitized mask to the same individual each time. The process has increased employee acceptance of reusing what is normally a single-use item while ensuring its proper fit.
The Centers for Disease Control and Prevention has recommended strategies for conserving personal protective equipment (PPE), including decontamination and reuse of N95 masks. Almost half of the healthcare facilities in the United States have reported being nearly or completely out of N95 respirator masks, the Association for Professionals in Infection Control and Epidemiology has reported.
In late March, before the program began, Barnes-Jewish had a low inventory of N95 masks, or about a week’s worth, and no expectations for replenishment because of international shortages in hospital supply chains.
The process begins at the end of the shift, when personnel place their N95 mask in a Crosstex sterilization pouch made of breathable Tyvek by DuPont polyethylene fiber in their unit’s soiled utility room. On the other side of the sealed pouch, personnel write their name or employee ID number, hospital, department, and unit location and put the pouch in the soiled collection bin.
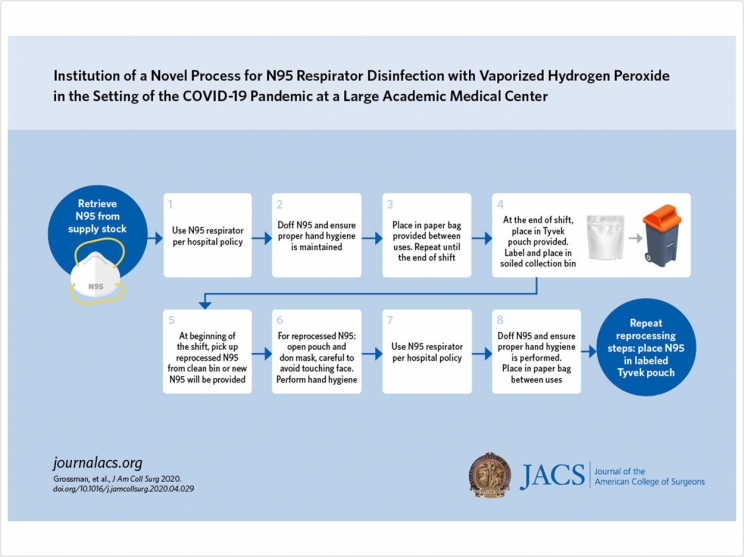
A designated worker wearing proper PPE collects the bins twice a day and takes them to a specially designed and sealed disinfection room that was built in four days. The pouches are then arranged, breathable side up, by clinical unit on wire racks. A Bioquell Z-2 hydrogen peroxide vapor generator that Washington University already owned to decontaminate equipment fills the room with the chemical.
After four and a half hours of disinfection, a worker moves the racks of masks to another area that has a fan to off-gas the hydrogen peroxide. The masks stay there until sensors record a zero reading. The pouches are returned to their respective units in a decontaminated bin, finishing a process that takes about seven hours.
Personnel can wear their mask up to three weeks because past studies show that disinfection more than 20 times could alter the fit of the mask. Since the program’s April 1 launch in the Barnes-Jewish emergency department, it has expanded to additional clinical departments and other hospitals in the system, which Pierce called “an immense achievement.”
The system is now disinfecting 240 N95 masks a day and could disinfect 1,500 masks daily. Without the disinfection program, Pierce said, the healthcare system would need to discard a substantial number of its respirator masks. Now, the hospitals have enough masks to last for weeks.
“This program is a welcome improvement for extended usage of N95s during the shortage that we are facing,” Pierce said.
Other hospitals facing mask shortages can reproduce the disinfection program if they bring together experts in environmental health and safety, medicine, and facility management, said senior author Shaina Eckhouse, MD, assistant professor of surgery at the Washington University School of Medicine and member of the team that developed the program.
“Having the infrastructure in place would improve the ease of deploying an N95 disinfection process,” said Eckhouse.
The study, “Institution of a Novel Process for N95 Respirator Disinfection with Vaporized Hydrogen Peroxide in the Setting of the COVID-19 Pandemic at a Large Academic Medical Center,” was published by the Journal of the American College of Surgeons.
Related Articles
ADHA Releases Guidance for Returning to Work
EPA and CDC Update Cleaning and Disinfection Guidance
Collaboration Developing 3-D Printed Reusable Filters for PPE












