INTRODUCTION
Immediate implant placement was first introduced in 1976 in Tübingen, Germany.1 This treatment modality has a high success rate that has been corroborated by multiple long-term studies and systematic reviews. The advancement of implant body designs, surface treatments, and other factors that improve and accelerate osseointegration has resulted in successful survival rates for immediate implants, which have reached 91% to 95% in studies.2-4 There are multiple advantages of immediate implant placement5: decreased healing time, fewer interventions, preservation of hard and soft tissues,6 and increased patient acceptance. Due to the reasons above, more and more practitioners are adopting immediate implant therapy into their arsenals, and implant companies are responding with better implant designs (tapered, aggressive threads) and surface treatments (improved osseointegration and bone-to-implant contact) that serve this purpose. Immediate implant therapy also has challenges and risks, such as decreased implant stability, prosthetically less-than-ideal placement, and unpredictable healing. Therefore, strict case selection criteria must be applied to achieve optimal results.7 This article highlights the use of a novel implant that allows familiarity to users, ease of placing it both in healed and immediate sites, increased primary stability, and faster osseointegration.
CASE REPORTS
Case 1: Maxillary Premolar Immediate Implant With Crestal Sinus Augmentation
A 61-year-old male patient presented to our clinic with the chief complaint of pain in the upper left quadrant. His health history was only remarkable for controlled hypertension, and the only relevant oral condition was bruxism. Clinical evaluation revealed a left maxillary second premolar that was fractured to the gumline (Figure 1). Radiographic examination revealed a 2-mm PARL at the apex of the tooth. In addition, the tooth’s apex was protruding into the maxillary sinus by 2 to 3 mm (Figure 2), which further complicated the difficulty level of the procedure. The prognosis of the tooth was questionable, and treatment options were presented to the patient. The patient elected for immediate implant therapy. On the day of surgery, anesthesia was performed via buccal and palatal infiltration using 3.4 mL of 4% Septocaine (Novocol Pharmaceutical). Phlebotomy was performed to obtain 3 vials of blood, which were used to produce a platelet-rich fibrin (PRF) membrane and sticky bone8 using a centrifuge and a 0.25-cm3 mix of A-Graft xenograft (Hiossen). The tooth was extracted atraumatically and completely. The intactness of the buccal plate was confirmed by direct vision and by running surgical instruments from the bottom of the socket to the most coronal portion of the buccal plate. No flap was elevated in order to minimize the damage to the buccal plate as a result of decreased blood flow. The intactness of the maxillary sinus was confirmed by direct observation of the sinus membrane and by irrigation of the socket with saline. Crestal sinus augmentation was performed using the CAS Kit (Hiossen),9 which has flat-end drills (Figure 3) that have depth stoppers (Figure 4) incrementally increasing the osteotomy depth by 1 mm.








Once the osteotomy was complete, the sinus membrane was elevated using hydraulic pressure via the same CAS Kit instruments. After sinus membrane elevation, a small portion of a collagen plug (Integra Miltex) was introduced to act as a cushion, and then the sticky bone was introduced into the sinus cavity under the elevated Schneiderian membrane. A 4.5- × 10-mm EK Implant (Hiossen) was placed using the implant motor at 25 N/cm2 and at 15 rpm. The depth and the hex position of the implant were finalized using the torque wrench. The final insertion torque was 35 N/cm2, and the resonance frequency analysis (RFA) values were measured at 70, 71 using a penguin-type RFA device (Integration Diagnostics). The gap between the implant and the buccal plate was also grafted with the sticky xenograft. The PRF membrane was used in a poncho style with a 5- × 5-mm healing abutment (Figure 5). The patient was dismissed in good condition, with a prescription for postoperative antibiotics and over-the-counter pain medications. Ten weeks later, the patient returned for an integration check. The soft tissue looked excellent around the healing abutment. The RFA was measured again using the IS4 device and Type 36 MulTipeg (Integration Diagnostics), and the values showed an increase to 78, 78. This, along with a percussion test and radiographs, confirmed osseointegration. A closed-tray impression coping was used to capture the position and the timing of the implant (Figure 6), and a screw-retained, final restoration was made from a prefabricated abutment and a monolithic zirconia crown. The definitive final restoration (Figure 7) was delivered successfully and torqued to specifications, and the access was obturated (Figure 8) using PTFE tape and TPH Spectra LV packable composite (Dentsply Sirona). The occlusion was checked and adjusted accordingly, the restoration surface was polished, and the patient was scanned for an occlusal guard using the wireless Medit i700 intraoral scanner. The final delivery radiograph showed an excellent fit of the restoration and crestal bone stability (Figure 9).
Case 2: Mandibular First Molar Immediate Implant
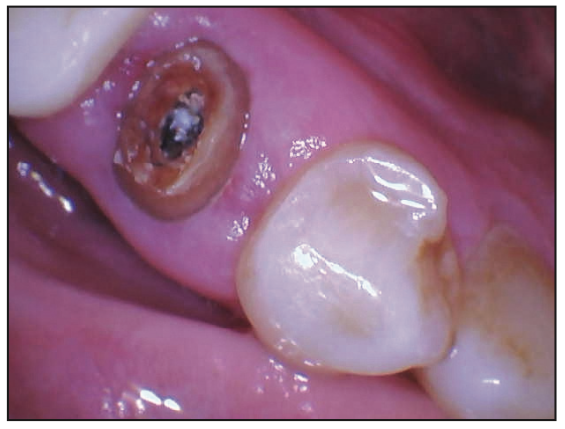
A 38-year-old female patient presented to our clinic with a fractured molar on the lower left side (Figure 10). The tooth had previously undergone root canal therapy and crown treatment 15 years prior. Clinically, the fracture was extensive, and the prognosis was poor (Figure 11). Medically, the patient was stable, ASA I, with no relevant conditions. Treatment options were explained to the patient, and the patient chose extraction and immediate implant therapy. Infiltration anesthesia was performed using 3.4 mL of 4% Septocaine via infiltration. Phlebotomy was performed to obtain 4 vials of blood for PRF and sticky bone protocols. A flap was not raised in order to minimize the damage to the buccal plate. A pre-extractive osteotomy technique was used to stabilize the implant drills (Figure 12). Once the osteotomy was complete, the remaining roots were extracted atraumatically, and a thin but intact buccal plate was confirmed visually and with surgical instruments. A 5- × 10-mm EK Implant was placed (Figure 13) using the implant motor, and the final depth and position were finalized using the torque wrench. The final placement torque was measured at 40 N/cm2, and RFA values were 70, 75. A 50/50 mix of SureOss Allograft (HansBiomed) and xenograft (A-Graft [Hiossen]) was mixed with the resulting PRF to produce sticky bone, which was placed in the extraction socket around the implant. A cytoplast collagen membrane (Osteogenics) and the PRF membrane were placed via poncho style with the healing abutment, and the area was sutured with 4.0 chromic gut sutures (Ethicon).







After 12 weeks of healing, the patient returned for the restorative steps. The RFA values had increased to 78 and 80, confirming osseointegration. A closed-tray impression coping was used to capture the position of the implant, and a final, screw-retained restoration was fabricated using monolithic zirconia and a customized, prefabricated abutment (Figure 14). The delivery process was uneventful, and the patient’s teeth were scanned for an occlusal guard using the wireless Medit i700 intraoral scanner. The follow-up bite-wing radiograph (Figure 15) showed stable crestal bone, and the clinical image captured the quality and health of peri-implant tissues (Figure 16).
DISCUSSION
Even though immediate implants were introduced in the mid-1970s, they truly became popular after the introduction of the All-on-4 concept10 by Dr. Paulo Maló in 1998. The concept included the immediate placement and loading of 4 implants to replace the teeth in each arch. This idea was commercialized in 2004, and since then, more than 250,000 patients have been treated using this trademark concept, and significantly more using the same idea of 4 to 6 implants to restore complete edentulism. Therefore, immediate implant placement is now a necessary tool in any actively practicing implantologist’s arsenal. A CBCT scanner (Planmeca) was used in the treatment planning for both cases. To be able to provide immediate treatment, the clinician not only needs the expertise but also the proper tools. Digital tools such as CBCT, intraoral scanners, and RFA devices can be used in the workflow from treatment planning to surgery and to final prosthetic rehabilitation. One of the most important tools in this process is the implant itself. The new EK Implant (Figure 17) from Hiossen provides multiple benefits and advantages: tapered design allowing for immediate placement, a hydrophilic surface, excellent primary stability, a high level of osseointegration and bone-to-implant contact, and strength. The nano-hydrophilic surface, which includes sand blasting, acid-etching and a low crystalline nano-hydroxyapatite, allows for enhanced osseointegration. The increased strength is due to the decrease of the connection size from 2.5 to 2.1 mm, which results in thicker implant walls and high strength, even in the 3.5- and 4-mm diameters. The implant has one prosthetic platform across the whole lineup, making prosthetics easier. One of the additional factors that makes this implant different is the special abutment-locking mechanism (Figure 18) that stabilizes the abutment during delivery and allows the clinician to tighten it using only one hand and with increased comfort. The special body and thread design (Figure 19) allow this implant to achieve high primary stability, even in immediate cases with sinus augmentation as seen in Case 1. The special surface treatment allows for faster osseointegration: In Case 1, the implant impressions were taken at 10 weeks post placement and delivered at 12 weeks. This shortens the treatment time and increases patient satisfaction. The initial placement stability and final osseointegration are also measured objectively using RFA and the Penguin-type device (Figure 20). Studies have shown that RFA values can be predictive of implant success and failure,11 therefore making RFA an indispensable tool in daily surgical and prosthetic protocols. In addition to getting good primary stability in soft maxillary bone, the EK implant has a very smooth insertion experience, allowing it to be placed in dense mandibular bone uneventfully without causing excessive pressure. The pre-extractive osteotomy technique used in the second case (Figure 12) was first described by Rodriguez-Tizcareño and Bravo-Flores12 in 2009, and then by Rebele et al13 in 2013. The protocol for this technique includes decoronating the tooth, then drilling the osteotomy through the roots of the tooth, and finally extracting the tooth before placing the implant. This technique significantly improves the stability of the drill and allows for more precise free-hand osteotomies. Both patients in this case series were fitted for occlusal guards, as studies indicate that implant failure can be minimized by multiple occlusal stabilization techniques, including the fabrication of occlusal guards.14 PRF was used in both cases to enhance the properties of the biological materials15 (allograft and xenograft) used for regeneration. A recent study on the effects of PRF on osteogenic differentiation of Schneiderian membrane-derived mesencymal cells showed that PRF used during sinus augmentation procedures accelerates bone healing and the quality of new bone.16,17 The author used analog impression techniques because, at the time of restoring these implants, this implant line had been recently introduced, and digital workflows were not yet available. Currently, the lineup of digital scan bodies and custom abutments has also been made available for this implant.




CONCLUSION
This article highlights the use of a novel implant design, which allows for easy placement in different types of bone, good initial stability, and reduced healing times. In a world where patients want results faster, immediate implant therapy has become a necessary tool in every implantologist’s arsenal and can allow for a much shorter healing time compared to delayed implant placement. Digital tools also further elevate the quality of immediate implant treatment, enhance patient outcomes, and become a strong practice builder.
REFERENCES
- Schulte W, Kleineikenscheidt H, Lindner K, et al. [The Tübingen immediate implant in clinical studies]. Dtsch Zahnarztl Z. 1978;33(5):348–59.
- Garcia-Sanchez R, Dopico J, Kalemaj Z, et al. Comparison of clinical outcomes of immediate versus delayed placement of dental implants: A systematic review and meta-analysis. Clin Oral Implants Res. 2022;33(3):231–77. doi:10.1111/clr.13892
- Thanissorn C, Guo J, Jing Ying Chan D, et al. Success rates and complications associated with single immediate implants: a systematic review. Dent J (Basel). 2022;10(2):31. doi:10.3390/dj10020031
- Ragucci GM, Elnayef B, Criado-Cámara E, et al. Immediate implant placement in molar extraction sockets: a systematic review and meta-analysis. Int J Implant Dent. 2020;6(1):40. doi:10.1186/s40729-020-00235-5
- Hamilton A, Gonzaga L, Amorim K, et al. Selection criteria for immediate implant placement and immediate loading for single tooth replacement in the maxillary esthetic zone: A systematic review and meta-analysis. Clin Oral Implants Res. 2023;34 Suppl 26:304–48. doi:10.1111/clr.14109
- Yu X, Teng F, Zhao A, et al. Effects of post-extraction alveolar ridge preservation versus immediate implant placement: A systematic review and meta-analysis. J Evid Based Dent Pract. 2022;22(3):101734. doi:10.1016/j.jebdp.2022.101734
- Morton D, Wismeijer D, Chen S, et al. Group 5 ITI Consensus Report: Implant placement and loading protocols. Clin Oral Implants Res. 2023;34 Suppl 26:349–56. doi:10.1111/clr.14137
- Dohan DM, Choukroun J, Diss A, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(3):e37-e44. doi:10.1016/j.tripleo.2005.07.008
- Kim YK, Cho YS, Yun PY. Assessment of dentists’ subjective satisfaction with a newly developed device for maxillary sinus membrane elevation by the crestal approach. J Periodontal Implant Sci. 2013;43(6):308–14. doi:10.5051/jpis.2013.43.6.308
- Maló P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5 Suppl 1:2-9. doi:10.1111/j.1708-8208.2003.tb00010
- Baltayan S, Pi-Anfruns J, Aghaloo T, et al. The predictive value of resonance frequency analysis measurements in the surgical placement and loading of endosseous implants. J Oral Maxillofac Surg. 2016;74(6):1145–52. doi:10.1016/j.joms.2016.01.048
- Rodriguez-Tizcareño MH, Bravo-Flores C. Anatomically guided implant site preparation technique at molar sites. J Implant Dent. 2009;18(5):393-401. doi:10.1097/ID.0b013e3181b4b205
- Rebele SF, Zuhr O, Hürzeler MB. Pre-extractive interradicular implant bed preparation: Case presentations of a novel approach to immediate implant placement at multirooted molar sites. Int J Periodontics Restorative Dent. 2013;33(1):88-95. doi:10.11607/prd.1444
- Lobbezoo F, Brouwers JE, Cune MS, et al. Dental implants in patients with bruxing habits. J Oral Rehabil. 2006;33(2):152–59. doi:10.1111/j.1365-2842.2006.01542.x
- Stumbras A, Kuliesius P, Januzis G, et al. Alveolar ridge preservation after tooth extraction using different bone graft materials and autologous platelet concentrates: a systematic review. J Oral Maxillofac Res. 2019;10(1):e2. doi:10.5037/jomr.2019.10102
- Wang J, Sun Y, Liu Y, et al. Effects of platelet-rich fibrin on osteogenic differentiation of Schneiderian membrane derived mesenchymal stem cells and bone formation in maxillary sinus. Cell Commun Signal. 2022;20(1):88. doi:10.1186/s12964-022-00844-0
- Castro AB, Meschi N, Temmerman A, et al. Regenerative potential of leucocyte- and platelet-rich fibrin. Part B: sinus floor elevation, alveolar ridge preservation and implant therapy. A systematic review. J Clin Periodontol. 2017;44(2):225–34. doi:10.1111/jcpe.12658
ABOUT THE AUTHORS
Dr. Boyer graduated from the University of California, Los Angeles (UCLA) School of Dentistry in 2008 and completed 2 GPR training programs at Cedars Sinai Medical Center and the VA Healthcare system, where he received advanced training in oral and maxillofacial surgery, complex and comprehensive treatment planning, and the placement and restoration of dental implants. He has been in private practice in Los Angeles since 2010. He is a faculty member at the UCLA School of Dentistry, where he teaches dental students and residents in the Advanced Education in General Dentistry program. In addition, he teaches dental implant CE courses nationally on dental implant surgery and restorations, guided surgery, crestal sinus lifts, immediate implants, overdentures, digital dentistry and intraoral scanning, implant stability, and RFA. Dr. Boyer has also trained at the UCLA Dental Implant Continuum, which is based on scientific research, current standards and protocols, and cutting-edge research and technology. In 2020, Dr. Boyer was invited to be one of 4 investigators in a 5-year, worldwide multicenter ceramic implant osseointegration and stability study led by the International Academy Of Ceramic Implantology (IAOCI) and the Zirconia Implant Research Group. He was recently appointed a board member of the IAOCI. He can be reached at dentist@ucla.edu.
Dr. Ji obtained her PhD in 2017 at the UCLA School of Dentistry. Her research involves oral health and innovative methodologies for detecting cancer cells of the head and neck tissues at early stages. Dr. Ji is an author of numerous primary research papers, book chapters, and peer-reviewed articles, which are available in various publication journals (eg, PLOS). In 2022, Dr. Ji graduated from the UCLA School of Dentistry with a DDS degree and joined Elite Dental Implant Center as an associate dentist. Dr. Ji practices placement and restoration of dental implants in addition to comprehensive treatment planning of complex cases. She can be reached via email at gracejiddsphd@gmail.com.
Disclosure: Dr. Boyer regularly lectures for Hiossen, Inc; has lectured in the past for Osstell; and has received an honorarium for writing this article. Dr. Ji has no disclosures.



