INTRODUCTION
A non-duchenne smile is evaluated in 3 parts: the teeth, the lip framework, and the gingival scaffold.1
The teeth should be of the appropriate size, shape, and visibility in the smile to be attractive. There should be no visible discoloring, and the teeth should appear to be uniform when evaluating contralateral positioning within the arch.
The ideal lip framework should have the upper lip within 1 mm of the gingival crest of the maxillary central incisors or with maximal coverage of 1 mm. The lower lip should follow the curvature of the maxillary arch smile and have the incisal edges just touching the vermillion border of the lower lip throughout the smile when done broadly.
The gingival scaffold should maintain the teeth in a healthy condition and mimic each side of the smile identically to give an aesthetic proportion to each side of the smile. It is essential to have a healthy band of attached tissue around the necks of the teeth.
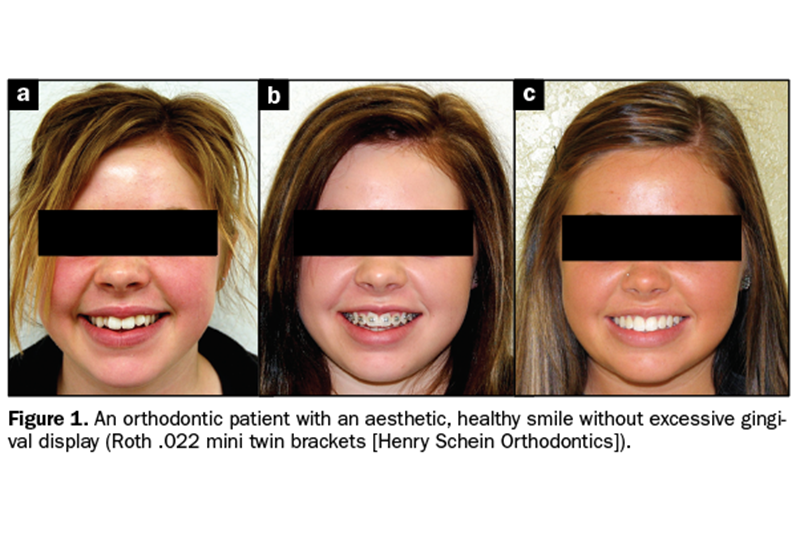
The overall appearance should be one of harmony and balance, with the dentist’s goal to improve on that harmony by either increasing or decreasing the appearance of gingival tissue and teeth in the smile (Figure 1).
Disharmony
A gummy smile, or a smile that has excessive maxillary gingival display, is traditionally a cosmetic concern when the patient becomes aware of it and asks if there is anything that can be done to improve his or her smile. The practitioner needs to be thorough in evaluating the patient to include the patient’s goals, expectations, and restrictions. Typically, many patients will decline a large-scale orthognathic solution to reduce gingival display unless they are already considering orthodontic care.
Determining the best way to reduce the level of gingival display is done by evaluating the cause of the display, which can be vertical maxillary excess, delayed apical migration of the gingival margin, a hypermobile lip, and/or a short upper lip.
Gingival display in excess of 2 mm above the gingival margin is not uncommon, with more areas showing greater than 4 mm of tissue above the cervical tooth margin in a broad smile.
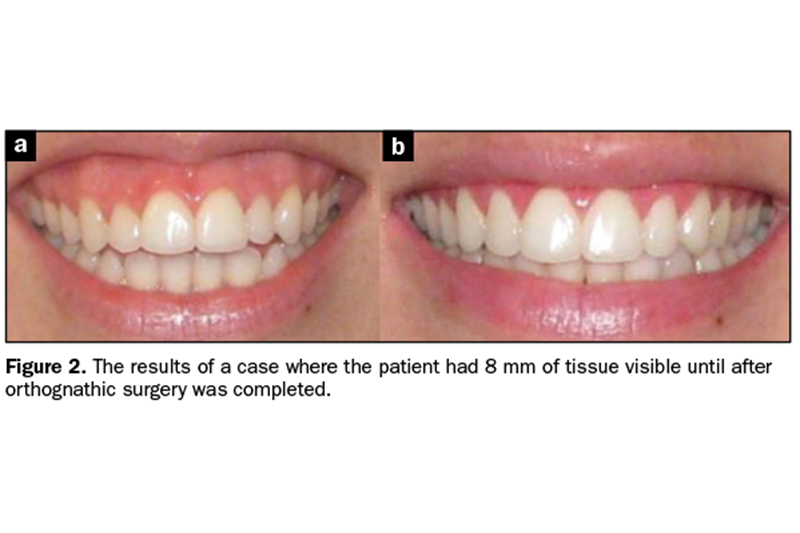
Cases with 8 mm or more of excess gingival tissue showing are best treated with orthognathic surgery due to vertical maxillary excess1 (Figure 2). New modalities with temporary anchorage devices (TADs) are less invasive and show promising improvements in cases that were previously only treatable with orthognathic surgery. For those patients who are intolerant of or financially unable to handle orthognathic surgery, TADs are a viable option.2
Hypermobile upper lips are more common than altered passive eruptions and orthognathic cases regarding the causes of excessive gingival display and provide the easiest surgical means of treatment.3,4
Hypermobile upper lips can be treated successfully with lip repositioning.5,6 Lip repositioning is meant to limit the actions of the elevator smile muscles. The zygomaticus major, levator anguli oris, orbicularis oris, and levator labii superioris all affect the smile.
The muscles within the oral cavity provide the greatest movement of the lip and form the ring of muscular fibers called the orbicularis oris. Partial myectomy of this muscle can help reduce relapse and is recommended as well as restrictive suturing of the fibers to allow partial atrophy. The Botox test will show if it would be a helpful adjunct to surgery. Restriction of the smile muscles helps reduce the excessive gingival display. By removing a strip of mucosa superiorly from the junction of the attached mucosa, the amount of muscular movement can be reduced significantly.
Treatment outcomes of gummy smiles with extraoral or intraoral causes have been well documented. Guidelines are essential to share with potential patients. Higher success rates occur when staying within guidelines (see Table 1).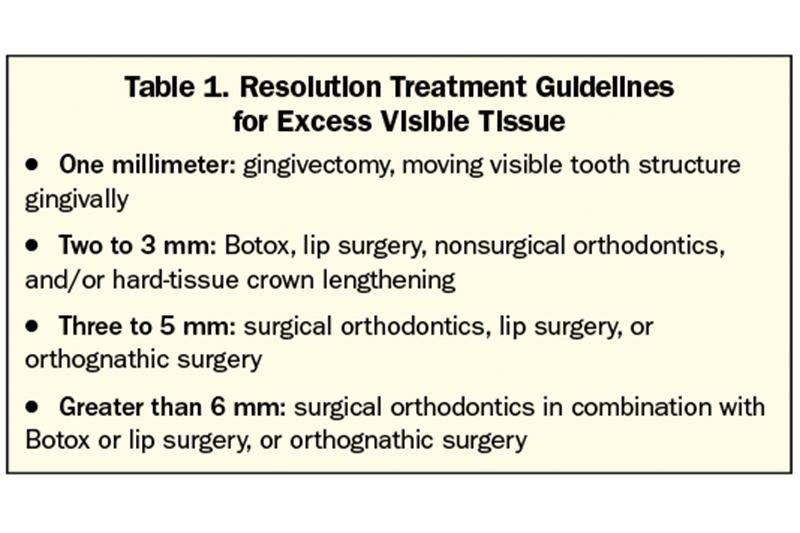
CASE REPORTS
Orthognathics and Orthodontics
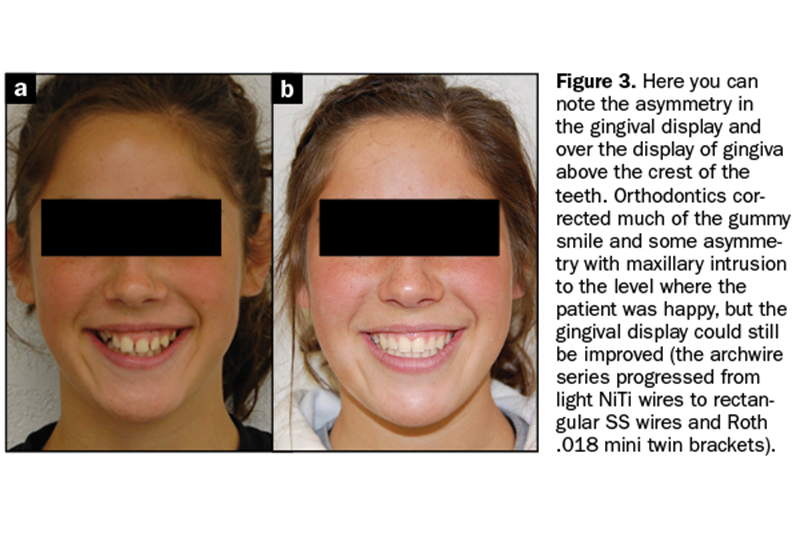
Figure 3 shows the asymmetry in the gingival display and over the display of gingiva above the crest of the teeth. Orthodontics corrected much of the gummy smile and some asymmetry with maxillary intrusion to the level where the patient was happy, but the gingival display could still be improved. We used an archwire series progressing from light NiTi wires to rectangular SS wires and Roth .018 mini twin brackets (Henry Schein Orthodontics).
Patient evaluation after treatment revealed that:
1. The patient’s left side would be better off treated with TADs, as her teeth were impacting unilaterally as part of orthodontic treatment with a prolonged time frame and increased cost. The patient’s parent refused that option, likely for good reason considering compliance was not ideal, and prolonged treatment would likely have increased complications.
2. Her crowns were clinically short, so the next step could be the placement of veneers since there would be no encroachment on the biological width due to the use of orthodontics to move the bone with the tissue.
3. Botox or lip repositioning were also viable alternatives since the incisal edges followed the lower lip.
4. Individual gingivectomies would be helpful because of tissue overgrowth due to oral care during orthodontic treatment. The patient and the parent also denied this option.
Patient motivation, timeframes, and finances often determine the final outcome of cases, so a thorough discussion must occur before beginning.
Temporary Anchorage Devices
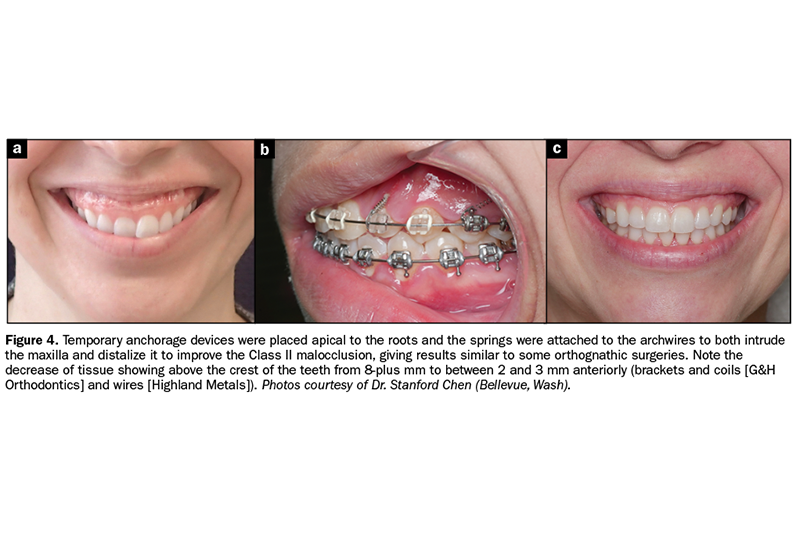
TADs are typically applied apically to the roots of the teeth to be intruded if possible. Complications include roots hitting the devices as they move apically, gingival overgrowth over the TAD, and loss of the TAD due to patient noncompliance or problematic force vectors.
Patient evaluation after treatment revealed that:
1. Results were dramatic, and again, the patient was very happy, but an ideal smile was not achieved based on the initial criteria documented (Figure 4).
2. Orthognathic surgery would have been required to get coincident midlines.
3. Since there was 2 to 3 mm of anterior gingival display progressing to nearly 6 mm posteriorly, the patient would still have benefited from any of the options within those guidelines if chosen.
4. When a dramatic improvement like this occurs, the patient rarely feels the need to improve to an ideal result, which is why expectations need to be discussed before treatment begins.
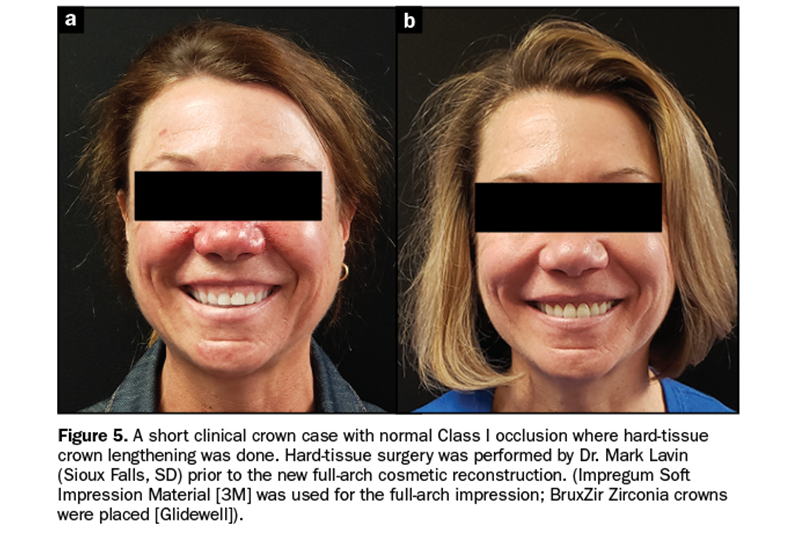
Hard-Tissue Crown Lengthening
Patient evaluation after treatment revealed that:
1. The patient’s gingival display was reduced from 6 mm to approximately 2 mm anteriorly through hard-tissue crown lengthening and prosthetic crowns (Figure 5).
2. Muscular contraction of the upper lip was evident, and either Botox or lip repositioning would be able to yield an ideal result. It is possible to find out how good the results of this would be by doing the “Botox test” and then waiting 2 weeks to see the outcome.
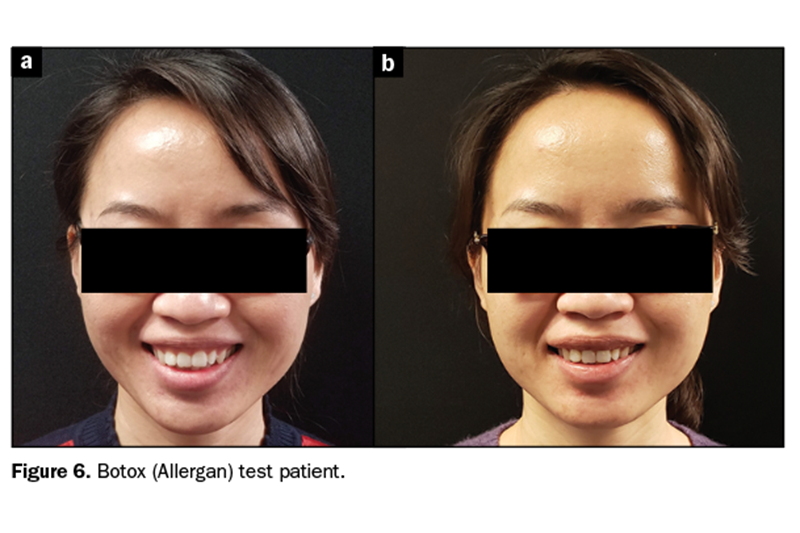
Botox Test
The Botox text is performed by depositing up to 6 units of Botox in the upper muscles of the lip. In this case, less is more. It is better to start with 1 or 2 units per side and wait than to do more in case you do it poorly, which is common with inexperienced users. If you do it poorly, it does affect the cosmetic nature of the patient’s normal smile, but you will have to wait up to 4 months before you can begin treatment.
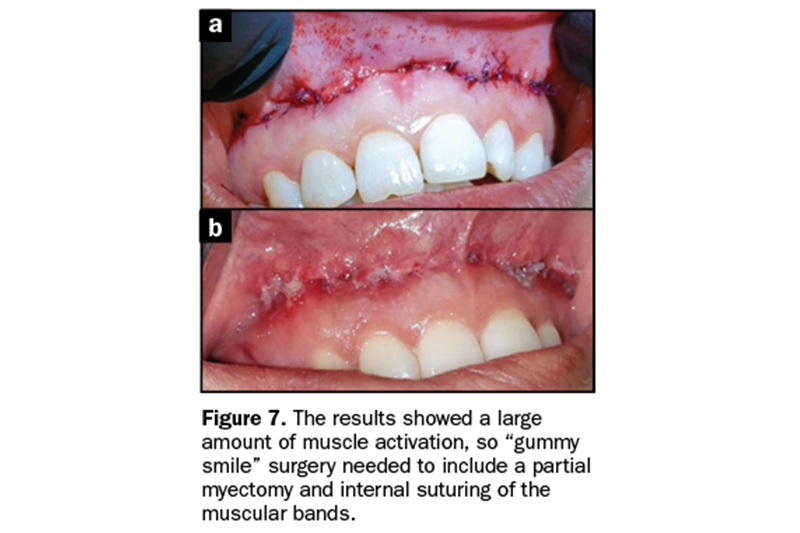
Figure 6 shows results with Botox alone to test how much of the treatment was muscle pull, which may cause relapse. Results showed a large amount of muscle activation, so “gummy smile” surgery would need to include a partial myectomy and internal suturing of the muscular bands (Figure 7) or the patient’s continuous use of Botox.
Gummy Smile Surgery With a Hypermobile Lip
A partial Myecotomy was performed with multiple sutures placed tightly around remaining muscle fibers during surgery. The day of surgery included 60 internal sutures and 12 external sutures using 5-0 polydioxanone sutures. Polydioxanone is a monofilament that wicks bacteria and self-dissolves slowly over time.
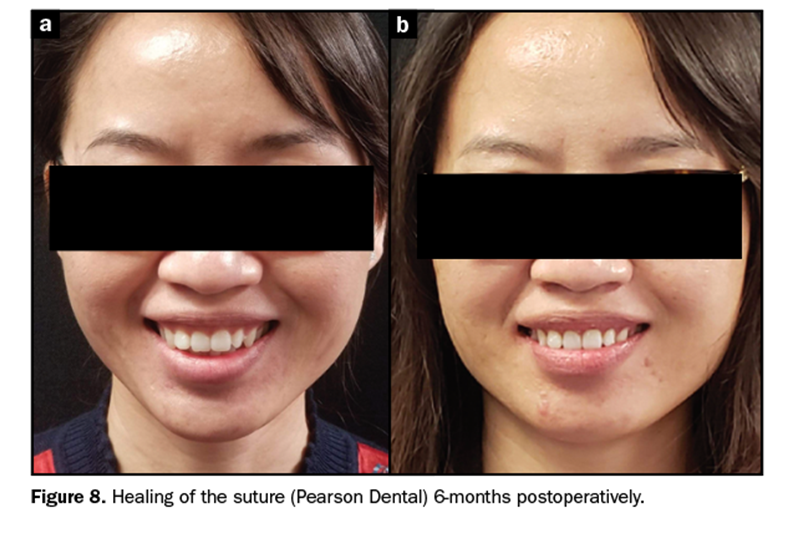
The results were the same as after the Botox test was performed and stable after 6 months when all the tissues were fully healed and the musculature re-established (Figure 8).
DISCUSSION
In the cases of gummy smiles in which there is the presence of short clinical crowns due to delayed/altered passive eruption, consideration should be given to doing hard-tissue crown lengthening. This assumes that biological width can be re-established further apically without tooth mobility and with stability. In cases with the presence of long clinical crowns, however, lip repositioning may be a treatment of choice.
Different techniques have been tried by the author of this article and his peers. For long-term stability and success, the author recommends:
1. Considering tissue elasticity in lip repositioning, which will predict the possibility of relapse in the future. The higher the amount of elasticity, the higher the probability of relapse.
2. Considering using Botox as a diagnostic tool to see if the muscles play a large or small role in the mobility of the lip prior to surgery. Use 2 units spread out on each side and take photos. See the patient again in 2 to 3 weeks and retake the photos. If the gingival display is resolved, you need less removal of tissue and more muscular resectioning and suturing internally for long-term success.
3. Careful measurement of the gummy smile (exposed gingiva) in order to calculate the amount of reduction in both surgical procedures of aesthetic crown lengthening and lip repositioning, which is important on both sides since they are rarely identical.
4. Evaluating the symmetry of the smile-line in case there is a need for correction on one side. Different amounts frequently need to be removed from each side to have a uniform final result since asymmetry is common.
5. That in lip repositioning procedures, the incision should be at the mucogingival junction and not within the mucosa alone, or high amounts of elasticity will remain, which will increase the likelihood of relapse. Suturing mucosa to mucosa increases the chance of relapse. The mucosa needs a firm stopping line, which is the demarcation of the attached tissue.
6. That internal sutures are more comfortable to the patient and less likely to come loose during healing. Long-term, resorbable, monofilament sutures that resorb over 2 months’ time work well to hold longer while tissues and musculature mature to their final positions. The author’s previous use of gut sutures increased complications and relapse because they dissolved too early. Polygylactic acid sutures lasted longer but attracted plaque and bacteria, which delay and worsen healing. Polydioxanone (PDO) has provided the ideal self-cleaning, long-term, self-resorbable suture for this procedure, in the author’s opinion. Using 3-0 for strength is useful internally for the muscles, and 5-0 is pliable and good when many sutures are required and when minimal scarring is required.
7. Dissecting thoroughly to the musculature and creating a large enough flap for visualization. Muscles must be managed by release, partial split-thickness resectioning and suturing internally for long-term success. It is essential to weaken but not cut through the musculature. Suturing it tightly together strengthens it while healing without allowing complete loss of function.
8. When considering gingivectomy to increase the length of the incisor appearance, do not plan on getting more than 1 mm of long-term results. When greater amounts are removed, it can be considered temporary due to biological width. Regrowth of the tissue to re-establish biological width occurs over time. For permanent lengthening of a short, squat-appearing incisor, hard-tissue crown lengthening is required. If restorative components are added over 1 mm of height, some additional gains can occur due to the biological width being forced apically. The tissue may appear red or bulbous during new biological width formation in the short term. Only minor invasions of the biological width are possible. No more than 2 mm of gain should be considered, or the results will not be controllable or repeatable. Hard-tissue crown lengthening is always preferred to properly preserve the biological width.
CONCLUSION
Improved reduction of gingival display plays a role in a cosmetic smile by improving the gingival scaffold and lip framework. There is a high degree of happiness in patients who undergo the surgery in terms of results and decreased morbidity compared to those who have orthognathic surgery. Long-term stability has always been a concern. With poor planning and case reports, soft-tissue surgery procedures have shown short-term stability with some long-term issues. By following the author’s suggestions and guidelines, long-term results can be better achieved, and existing cases can be improved.
Excessive gingival display is a frequent cosmetic concern for patients. Patients most often present with greater than 4 mm of excessive gingival display caused by hypermobile lips. Multiple options are possible for correction. Hypermobile lip surgery can be effective and has good long-term results when performed correctly.
References
1. Garber DA, Salama MA. The aesthetic smile: diagnosis and treatment. Periodontol 2000. 1996;11:18-28. doi:10.1111/j.1600-0757.1996.tb00179.x
2. Lee KJ. Chapter 58: The Application of TADs for Gummy Smile Correction. In: Park JH, ed. Temporary anchorage devices in clinical orthodontics. John Wiley & Sons. 2020.
3. Andijani RI, Tatakis DN. Hypermobile upper lip is highly prevalent among patients seeking treatment for gummy smile. J Periodontol. 2019;90(3):256-262. doi:10.1002/JPER.18-0468
4. Rosenblatt A, Simon Z. Lip repositioning for reduction of excessive gingival display: a clinical report. Int J Periodontics Restorative Dent. 2006 Oct;26(5):433–437.
5. Simon Z, Rosenblatt A, Dorfman W. Eliminating a gummy smile with surgical lip repositioning. J Cosmet Dent. 2007;23:100-108.
6. Dutra CR, Primo PP, de Freitas DS, et al. Comparison of Botulinum Toxin and Orthognathic Surgery for Gummy Smile Correction. Open Dentistry Journal. 2020. 14:416-420. doi:10.2174/1874210602014010416
Dr. Brower graduated with honors in 1997 from the University of Minnesota and received advanced training in surgery through the US Army and beyond. He has more than 20 years of private practice experience as an owner and is a frequent teacher of advanced surgical procedures with a number of different periodontists and oral surgeons. He is a lifetime member of the American Orthodontic Society and has been published multiple times. His daughter, Morgan Brower, attends Creighton School of Dentistry in Nebraska He can be reached at browerj@gmail.com or at the website getdentaltraining.com.
Disclosure: Dr. Brower reports no disclosures.