INTRODUCTION
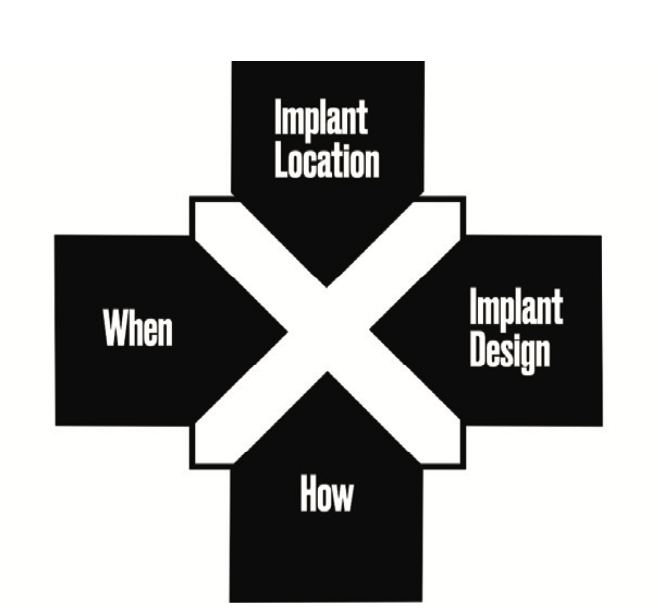
When it comes to implant dentistry, it is proposed that there are 4 key treatment axioms that should be prioritized for long-term success: implant location, design, guided surgery, and timing (Figure 1). Together, these 4 core principles form the cornerstones of dental implantology and help to ensure successful implant solutions with fewer complications. Each factor is important on its own, but when taken together, they provide an optimization-comprehensive approach to tooth replacement therapy. In this article, we will explore how each of the 4 core principles work together to promote longevity and success in implant dentistry.
LOCATION
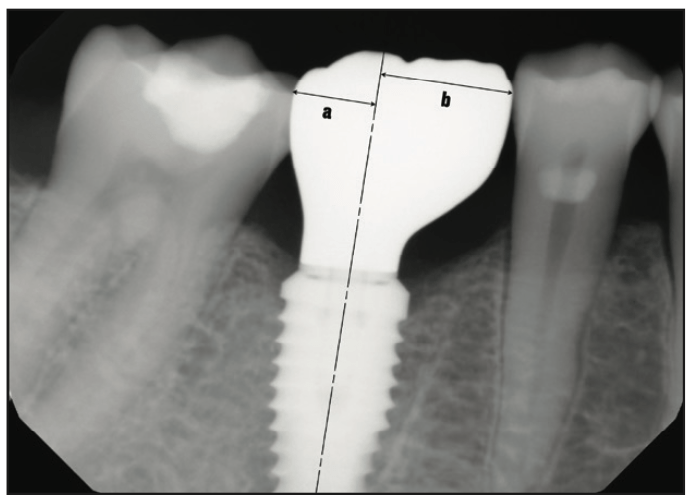
Positioning a dental implant correctly is the key to successful long-term outcomes. An incorrectly placed dental implant can lead to several biological and mechanical complications, resulting in increased stress and cost for both the patient and the dentist. When implants are positioned incorrectly, they can cause a multitude of problems, such as being placed in poor quality or quantity of bone, resulting in a fenestration or lack of osseointegration.1 Poor placement may also lead to aesthetically unappealing FP2 solutions as well as create cantilevers that produce food traps and decrease patient satisfaction (Figures 2 and 3).2 In addition, there may be insufficient hard and soft tissue on the labial side, leading to displeasing discoloration of the gingiva.3 To avoid these issues, it is essential to ensure proper implant placement from the start.

Implant Loading
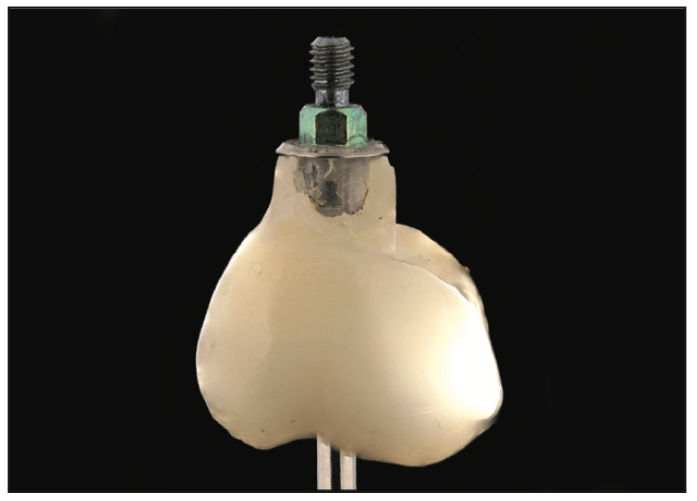
When placing dental implants and their components, it is essential for them to be loaded axially so that the reactive force is directly beneath the applied force.4 If this vertical line of balance between forces is not achieved, the resulting cantilever prosthesis will generate rotation forces on the system. These rotational forces, called bending moments, could potentially lead to prosthetic fracture, dental implant breakage, de-cementation, abutment fracturing, abutment screw loosening, and/or fracture (Figure 4).5,6
Site Selection
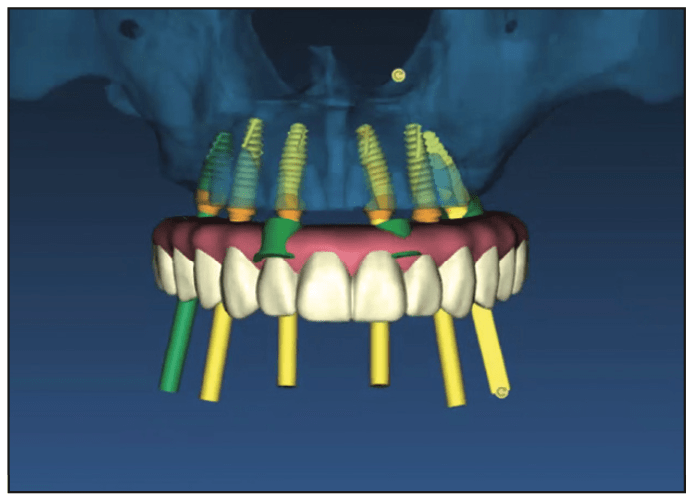
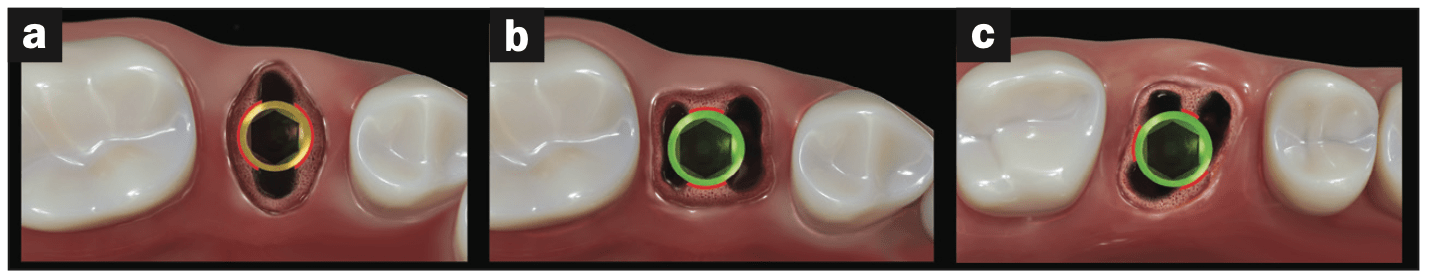
To identify the ideal site for an implant, 3D radiographic imaging (iCAT FLX [DEXIS]) and an optical intraoral scan (TRIOS 3 [3Shape]), along with treatment planning software (Implant Studio [3Shape]), should be used. This prosthodontic-driven virtual approach allows dental clinicians to visualize how a prosthetic will look and function in its final location before live surgery begins, eliminating any potential guesswork associated with the image distortion that flat, 2D radiographs create.7 Utilizing these resources before surgery can help reduce surprises during the surgical procedure and ensures greater accuracy when placing dental implants, ultimately leading to higher success rates in the long run (Figure 5).8
IMPLANT DESIGN
The design of the dental implant is critical to its success, as it must be constructed from durable materials with micro and macro features that ensure safety and efficacy (Tapered Pro [BioHorizons]). Implant design should account for not only the physiological requirements of the patient and prosthetic solution but also the repetitive biomechanical demands of everyday use. A dental implant must be designed to withstand cyclic chewing forces, torsional loads, and occlusal pressures over a long period of time without fatigue, failure, or fracture. The toughest dental implants are made from titanium alloy, which is biocompatible, lightweight, and strong enough to provide long-term durability. Additionally, at the micro level, dental implants should have a rough surface to promote bone growth and adhesion during the osseointegration process.9 Furthermore, dental implants should incorporate macro features, such as threading on their exterior surfaces for increased stability and retention of the prosthetic solution when compared with smooth cylinders. Tapered implants can be placed in tight locations and create good primary stability because of their wedge effect. When all of these and other factors are considered during dental implant design, it ultimately leads to higher success rates and increased longevity.
Materials
When it comes to dental implants, titanium is the most common choice of metal due to its biocompatibility.10 Grade 4, commercially pure titanium can be used, but it is not as strong as a medical Grade 23 titanium alloy, such as Ti-6AI-4V ELI.11 This titanium alloy has been shown to be nearly 40% stronger than basic Grade 4 titanium in terms of yielding and fatigue resistance. While pure titanium will remain firmly in place over time, a titanium alloy-constructed dental implant can prove much more durable and long-lasting with fewer complications than pure titanium alone.12 It is also non-corrosive and biocompatible, which ensures that dental implants made of this material will integrate well into the surrounding tissue without causing any irritation or damage.13 The combination of strength, flexibility, and biocompatibility makes this alloy an ideal choice for dental implants that need to last long-term with minimal maintenance worries.
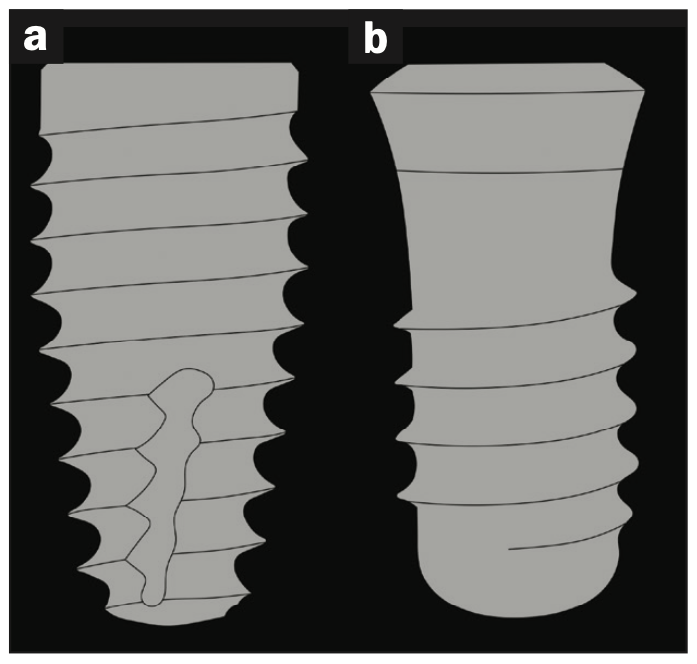
Thread Design
When selecting the most appropriate implant design, biomechanical interactions between the implant and bone must be considered. Bone can withstand compression forces proficiently, yet bone is susceptible to tensile and shear forces.14 Therefore, after a device is implanted in the body and integrated, a prudent approach would be to apply compressive loads on the bone instead of tension or shear stress for optimal performance during daily use. The V-shaped thread creates more shear force on the bone than a square-shaped thread (Figure 6).15 However, since a self-tapping V-thread is easier to install and does not require an additional tool like a bone tap, many opt for this design. The buttress thread (Tapered Conical Pro [BioHorizons]) represents an appealing compromise between the 2 shapes; with its flat side facing apically toward the bone, less shear stress is applied while still providing installation without requiring extra tools.
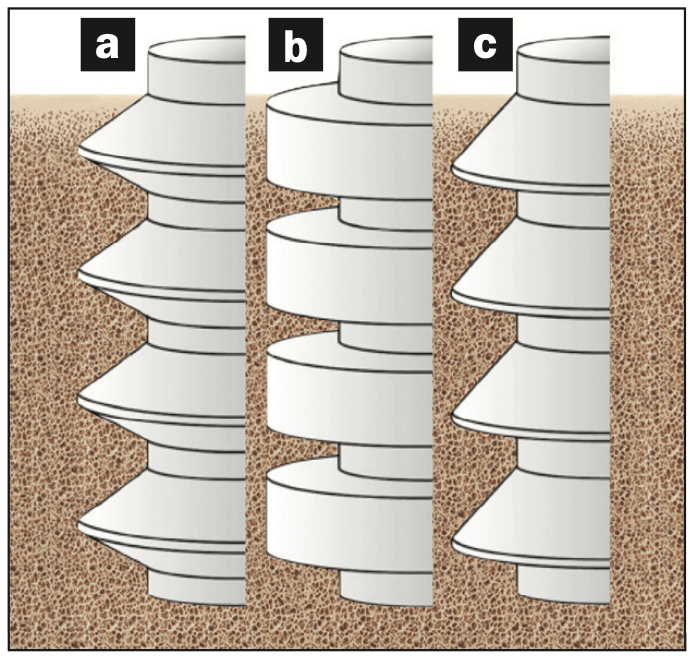
Thread Pitch
Both the shape of an implant and its number of threads play a crucial role in its long-term success.16 According to the author’s article published in The Journal of Oral Implantology, the “Five Thread Guideline” is a principle used by engineers that helps predict the likelihood of primary implant stability in fresh extraction sites when 5 threads are engaged with native bone, consequently resulting in good primary stability.17 After numerous calculations and experiments, engineers (Spiralock [STANLEY Engineered Fastening]) have discovered that the minimum number of threads needed to effectively hold a clamp force is 5.18 This rule applies to both nuts and bolts as well as implant threads to bone. Most forces sustained by the bone are in the first 5 threads closest to where the force is being applied.19 For a secure and stable fit, at least 5 threads should be engaging 2 points of contact on the bone. While certain sockets may provide more contact points for the threads (such as those found in maxillary first molars), even teeth with just one root, like mandibular incisors, can still offer satisfactory stability when connected to only 2 anchor points (Figure 7). With an implant thread pitch of 1 mm, just 5 mm of implant length needs to interlock with the native bone to engage 5 threads. This stands in stark contrast to a 2-mm coarse-pitched implant, which necessitates that the implant’s entire 10-mm length must be in contact within native bone—making this design inappropriate for fresh extraction sites as it is highly improbable for total bone-to-implant contact in such situations (Figure 8).
GUIDES
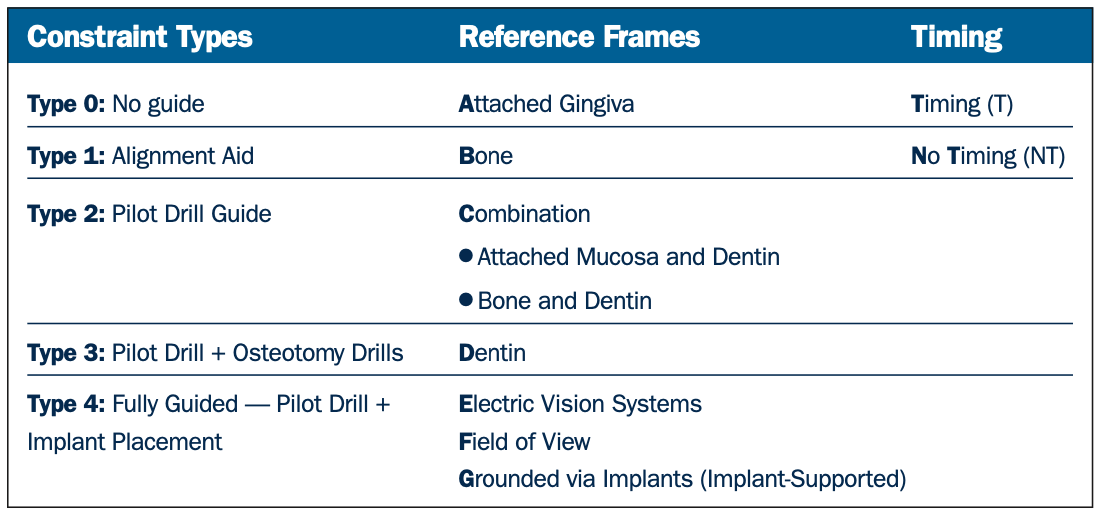
The use of surgical aids to help guide dental implants into the proper locations is a critical step in the process for long-term success. Different types of guides are available for different stages of implant placement and can be used either as visual aids or as physical constraints (Table 1).20 Type 0, or no guide, simply relies on the dental professional’s experience and skill alone to position the dental implant in the correct place. Type 1 is a visual guide that gives reference points and offers visuals that dental professionals can follow. Type 2 is a pilot drill guide, which offers guidance with predetermined drilling paths for more accuracy. Type 3 is an osteotomy guide, which requires custom fit guides to direct dental implants into bone with precision and accuracy. Lastly, type 4 fully guided surgery minimizes positional errors and helps reduce any risk of future complications. This procedure accounts for the non-homogeneous anisotropic nature of bone and offers greater control over dental implant placement by providing internal tolerances at 200 µm or less. By designing (Implant Studio [3Shape]), printing (Pro 2 3D printer [SprintRay]), and performing a fully guided dental implant surgery, dental professionals can ensure that their patients’ dental implants will be placed in their ideal prosthetic and biomechanical locations according to their specified plans, with minimal risk of deviation or misplacement.
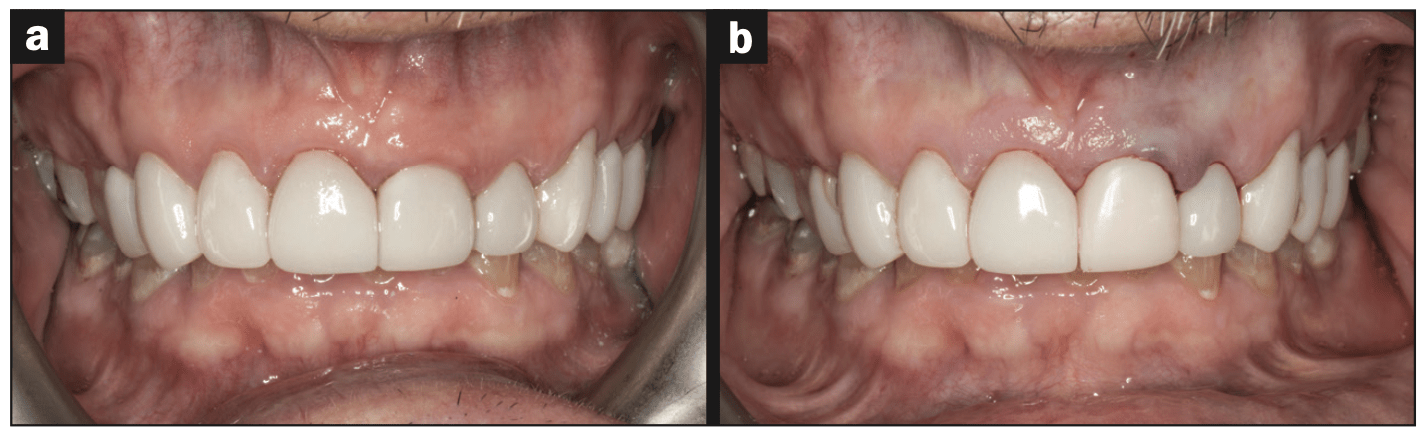
TIMING
The timing of dental implant placement is an important factor when considering long-term success, especially in aesthetic zones where maintaining hard- and soft-tissue architecture is preferred over re-creating it (Figure 9).21 Research has suggested that immediate dental implant placement without labial flap elevation, gap grafting, or provisionalization may be a more successful approach in achieving desirable results.22 The utilization of a fully guided type 4 surgical guide is essential during this procedure to ensure the best possible implant location is achieved. Not only does an immediate implant placement reduce the risk of bone loss, but it also provides a more efficient system for both the patient and dental professional alike. The traditional dental implant procedure can take up to one year from initial extraction to delivery of the final prosthesis. This necessitates multiple appointments, incurring additional costs and creating inconvenience for the patient. Immediate dental implants can reduce this timeline significantly, allowing patients to walk away with their final prosthetic solutions (Prime Zirconia [Ivoclar]) after only 3 months of healing and 2 additional weeks of final prosthetic fabrication (CMR dental lab). This encourages an optimal experience for both parties involved as well as minimizes wait time for the final product while reducing any risks associated with bone loss. Additionally, patients can save time and stress by making fewer visits to the office due to this accelerated timeline.
CONCLUSION
The outcome of a dental implant tooth replacement solution is not reliant on one factor alone; clinicians should consider all aspects when planning for each patient. However, it is suggested that a weighted focus be allocated to these 4 key parameters: location, design, guides, and timing. When these requirements are met—including selecting the most suitable implant, placing it precisely in its optimized location, and utilizing a type 4 guided surgery at extraction time—the dental professional can be confident that his or her patients will experience optimal results for many years to come.
REFERENCES
- Le B, Nielsen B. Esthetic implant site development. Oral Maxillofac Surg Clin North Am. 2015;27(2):283-311. doi:10.1016/j.coms.2015.01.009
- Fürhauser R, Florescu D, Benesch T, et al. Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin Oral Implants Res. 2005;16(6):639–44. doi:10.1111/j.1600-0501.2005.01193.x
- Cooper LF. Objective criteria: guiding and evaluating dental implant esthetics. J Esthet Restor Dent. 2008;20(3):195-205. doi:10.1111/j.1708-8240.2008.00178.x
- Chuan-Yi Su J-HF, Wang HL. The role of implant position on long-term success. Clin Adv Periodontics. 2014;4(3):187–93. doi:10.1902/cap.2013.120100
- Chrcanovic BR, Kisch J, Albrektsson T, et al. Factors influencing the fracture of dental implants. Clin Implant Dent Relat Res. 2018;20(1):58-67. doi:10.1111/cid.12572
- Kourtis S, Damanaki M, Kaitatzidou S, et al. Loosening of the fixing screw in single implant crowns: Predisposing factors, prevention and treatment options. J Esthet Restor Dent. 2017;29(4):233–46. doi:10.1111/jerd.12303
- Tolstunov L. Is implant dentistry a restorative discipline with a surgical component? A change of definition is proposed. J Oral Implantol. 2011;37(2):293–5. doi:10.1563/1548-1336-37.2.293
- Tallarico M, Meloni SM, Park C-J, et al. Implant fracture: A narrative literature review. Prosthesis. 2021;3(4):267–79. doi:10.3390/prosthesis3040026
- Jimbo R, Albrektsson T. Long-term clinical success of minimally and moderately rough oral implants: a review of 71 studies with 5 years or more of follow-up. Implant Dent. 2015;24(1):62–9. doi:10.1097/id.0000000000000205
- Liu X, Chen S, Tsoi JKH, et al. Binary titanium alloys as dental implant materials—a review. Regen Biomater. 2017;4(5):315–23. doi:10.1093/rb/rbx027
- Xi D, Wong L. Titanium and implantology: A review in dentistry. J Biol Regul Homeost Agents. 2021;35(Suppl 1):63-72.
- Stoichkov B, Kirov D. Analysis of the causes of dental implant fracture: A retrospective clinical study. Quintessence Int. 2018;49(4):279–86. doi:10.3290/j.qi.a39846
- Dias Corpa Tardelli J, Bolfarini C, Cândido Dos Reis A. Comparative analysis of corrosion resistance between beta titanium and Ti-6Al-4V alloys: A systematic review. J Trace Elem Med Biol. 2020;62:126618. doi:10.1016/j.jtemb.2020.126618
- Reilly DT, Burstein AH. The elastic and ultimate properties of compact bone tissue. J Biomech. 1975;8(6):393-405. doi:10.1016/0021-9290(75)90075-5
- Strong JT, Bidez MW, Nalluri P. Functional surface area: thread-form parameter optimization for implant body design. Compendium. 1998;19(3).
- Misch CE. Contemporary Implant Dentistry. 3rd ed. Mosby Elsevier; 2008.
- Stanley R. The five thread guideline: a new guideline for predicting primary stability with dental implants. J Oral Implantol. 2020;46(1):81–6. doi:10.1563/aaid-joi-D-19-00039
- Budynas RG, Nisbett JK, Shigley JE. Shigley’s Mechanical Engineering Design. 10th edition. McGraw-Hill Education; 2015.
- Bozkaya D, Muftu S, Muftu A. Evaluation of load transfer characteristics of five different implants in compact bone at different load levels by finite elements analysis. J Prosthet Dent. 2004;92(6):523–30. doi:10.1016/j.prosdent.2004.07.024
- Stanley RJ. A comprehensive classification system for dental implant surgical guides. Dent Today. 2022;41(3).
- Tarnow DP, Chu SJ. The Single-Tooth Implant: a Minimally Invasive Approach for Anterior and Posterior Extraction Sockets. Quintessence Publishing; 2019.
- Cosyn J, Eghbali A, De Bruyn H, et al. Immediate single-tooth implants in the anterior maxilla: 3-year results of a case series on hard and soft tissue response and aesthetics. J Clin Periodontol. 2011;38(8):746–53. doi:10.1111/j.1600-051X.2011.01748.x
ABOUT THE AUTHOR
Dr. Stanley is in private practice with his wife, Dr. Bobbi Stanley, in Cary, NC. Dr. Stanley co-founded the Stanley Institute with the sole mission of making dental implants easy. He uses his unique background in engineering and dentistry to help dentists painlessly master 3 key components of implantology: planning, placement, prosthetics, and maintenance. Dr. Stanley also invented Brite-gums, a cosmetic procedure to uniformly pinken one’s gums. Dr. Stanley can be found on social media @smileengineer and can be reached at drrobert@stanleyinstitute.com.
Disclosure: Dr. Stanley reports no disclosures.



