A variety of laser wavelengths have been investigated for use in medicine and dentistry as realistic alternatives to conventional approaches to the cutting or removal of tissue during surgery. This literature review is intended to assess the potential of the dental infrared Er:YAG laser for safe and reliable thermal mechanical ablation of osseous tissues in the oral cavity and to discuss the use of the Er:YAG laser for procedures involving the oral soft tissues and tooth enamel.
BACKGROUND
In 1917, Einstein published his theory of stimulated emissions of photons, hence providing future scientists with the basis for creating a functional laser.1 In 1960, Maiman created the first usable laser, which led to a search for possible medical applications for these devices.2 Physicians and dentists have looked to lasers as an alternative to conventional mechanical instruments as a means of performing less invasive surgical procedures. In dental surgery, cutting of alveolar bone has been a major focus of research. To effectively cut alveolar bone without the thermal necrosis caused by other laser systems, a laser that selectively targets the chromophore of water and not the extracellular bony matrix is required.
The electromagnetic energy emitted from a laser has unique characteristics that are fundamentally different from light energy emanating from a nonlaser source. All of the photons emitted from a laser are (1) coherent (moving in the same direction and phase) and (2) all of the same wavelength (color). This allows a practitioner to exert maximum power per unit area irradiated while simultaneously targeting a specific chromophore (tissue element) as an absorptive media for the unique wavelength of laser energy being used.
The Er:YAG laser at a wavelength of 2.94 µm has the highest specificity for water absorption of all the mid-infrared lasers.3 In the past, this wavelength has been specifically used for very accurate ablation and cutting in different disciplines, including ophthalmology, laryngeal surgery, and dermatology. Detailed histologic analyses of ablated tissue after irradiation with an Er:YAG laser have described well-defined cuts with very small zones of thermal necrosis not greater than 40 µm (40/1000ths of a mm). In comparison, the thermal necrosis zones caused by Er:YSGG and CO2 laser systems were approximately twice as large, and histological samples observed with argon and Ho:YAG lasers produced thermal tissue necrosis zones of 200 to 300 µm.4 Therefore, among the major clinical advantages of using the Er:YAG laser is its ability to ablate both hard and soft tissues with minimal thermal damage.5 Because of their unique absorption peak in water, Er:YAG-generated photons warrant strong consideration as a useful tool to cut mineralized biologic tissues such as natural tooth structure and bone.
Two important considerations for lasers that are highly specific for water absorption are thermal expansion and heat transfer through conduction. If these ideas are clearly understood, a clinician can maximize the desired effects while minimizing collateral tissue damage during laser irradiation.
ER:YAG INTERACTION WITH SOFT TISSUE
When using an Er:YAG laser in a pulsed mode with 200- to 400-microsecond pulse widths, 5 to 40 µm of thermal mechanical tissue ablation (tissue removal) with as little as 5 µm of residual thermal damage is generally observed for soft tissues. These characteristics result in a very narrow zone of thermal mechanical tissue ablation with minimal collateral thermal damage.6
Venugopalan et al7 described erbium tissue ablation in 1995. They surmised that to effectively cut or ablate human mucosa, the Er:YAG laser targets the chromophore of water selectively instead of the extracellular matrix of collagen. This produces an instantaneous vaporization of the water to a depth of about 4 µm per pulse. They observed that the mechanical integrity of the extracellular matrix (collagen) is not directly targeted when water is the dominant chromophore. Hence, to achieve tissue removal, the heated water (intracellular steam) expands, straining and later fracturing the matrix components (primarily collagen) in the extracellular environment.
With the Er:YAG laser optical energy, the infrared beam is converted to local thermal energy in a confined tissue volume, and this occurs in the target chromophore of water. The result of this absorption in a thin layer of tissue is instantaneous tissue degradation or ablation. Accompanying this is an explosive ejection of the degraded cellular components and heated vaporous material.8,9 Because Er:YAG energy has such a high absorption peak in water, the thermal damage to the tissue is minimized as the thermal mechanical ablation takes place (ie, there is no charring). Improved healing of the irradiated tissue is the result. Neev et al10 in a thermo-optical skin conditioning study, observed that less thermal damage means less collagen remodeling is necessary. With less collagen damage and remodeling, faster healing with minimal scarring of soft tissue is seen.
 |
 |
| Figure 1. Beginning Er:YAG incision for minimally invasive implant surgery. |
Figure 2. Completed Er:YAG Incision for minimally invasive implant surgery. |
With the largest absorption coefficient in water of all the mid-infrared lasers, the Er:YAG has a very small optical penetration depth in water (less than 1 µm).11 As a result, the tissue around the irradiated zone experiences only minimal damage, which is confined to 10 µm beyond the border of the tissue-beam interface. If the wavelength of the Er:YAG (2.94 µm) is compared to conventional dental diode soft-tissue lasers (810 nm to 980 nm), the depth of penetration per pulse with diodes is estimated to be greater by a factor of 104 (10,000x), or 4 cm.11 A diode laser is a solid-state laser with completely different chromophore targeting and absorption characteristics than the Er:YAG. Diode lasers have shorter wavelengths (800 or more nm versus 2.94 µm) and thus have high absorption peaks in melanin and hemoglobin. This will cause the laser energy to pass through the water and produce thermal haemostatic and necrotic effects much deeper in the tissues since the photons are absorbed by the tissue pigments. Hence, the Er:YAG laser is safer and more controlled for purposes of cutting but does not have good haemostatic properties.11 Procedures such as a gingivectomy, gingivoplasty, frenectomy, incision and drainage, and removal of a fibroma are easy to accomplish using the Er:YAG laser, but the haemostatic properties are considered marginal12 (Figures 1 and 2).
ERBIUM LASER EFFECTS ON TEETH
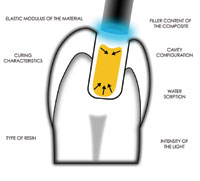
In 1997, the US Food and Drug Administration (FDA) approved the Er:YAG laser for caries removal, cavity preparation, and laser-etching of enamel.13 This is the most effective laser in the mid-infrared spectrum for the ablation of dental enamel, and the photobiology of the Er:YAG-enamel interaction has been defined.9,10,14 Water molecules within the prismatic enamel layer of a tooth make up only 4% of its chemical composition. However, they represent 11% of enamel’s total volume. As the laser energy interacts with the enamel matrix, water absorbs the laser energy and rapid vaporization of the water occurs. As this photothermal reaction takes place, the steam generated within the enamel is associated with a volumetric expansion within the enamel matrix. This in turn produces micro-evaporative explosions that result in a thermally driven, mechanical ablation of the tooth structure.14
 |
 |
| Figure 3. Er:YAG enamel ablation for cosmetic bonding. | Figure 4. Completed thermal mechanical ablation and etch accomplished with Er:YAG laser. |
The effect of water spray and thermal tissue effects with the Er:YAG laser on both hard tissues and dental materials were investigated and described by Wigdor, Visuri, and Walsh.15,16 They found that as long as enamel is continually hydrated with a water spray during the laser exposure (serving as a heat sink), there will be only a minimal increase in temperature of the enamel layers and deeper tissues. These data are clinically important. Friedberg et al17 reported on another FDA-approved laser for cutting of teeth, the Er:YSGG. They found that additional energy is required from the unit to initiate enamel ablation when the laser is propagated through an aerated mixture of water droplets. This method was found to attenuate the beam as opposed to the water being sprayed directly on the irradiated area of enamel and acting as a heat sink17 (Figures 3 and 4).
BACTERICIDAL EFFECTS OF THE ER:YAG LASER
A major advantage of the Er:YAG laser as compared to mechanical therapy for procedures on biologic tissues is the bactericidal effect of the laser. During the Er:YAG tissue interaction, the bacteria in the path of the beam are destroyed as the water within the bacterial cells undergoes the same instantaneous phase change (liquid to steam) as the water in the tissue matrix being ablated.18,19 The destruction of bacteria during treatment may be an important ancillary effect of the use of the laser. A study by Ando et al18 demonstrated the pronounced potential of the Er:YAG laser on periodontal bacteria even at low energy levels.
CURRENT MEDICAL APPLICATIONS OF ER:YAG LASERS FOR BONE
Er:YAG bony ablation has been successfully accomplished in a variety of clinical situations. In a review of the use of this laser for middle-ear ablation procedures, Frenz et al20 stated that otological surgeons have identified the advantages of this laser for osseous surgery. These are the water absorption characteristics of the wavelength and the precise bone ablation with minimal residual thermal energy. The histological data for Er:YAG lasers, when used by otological surgeons to perforate stapes footplate (osseous ear tissue) in surgical procedures, demonstrates that the lateral thermal damage associated with the bony cut was restricted to only 5 to 10 µm beyond the cuts.
When attempting to cut nasal bone with a laser, Truong et al21 described 2 specific criteria that should be met before a laser wavelength is chosen. These are rapid tissue ablation and an absence of visible char at the ablation site. They concluded that this laser produced an excellent result and further stated that the addition of a water spray on the area being irradiated during ablation resulted in the lowest level of char and presumably the lowest thermal damage to the tissue. It was also noted that as long as the surface of the ablated tissue remained moist with a water spray throughout the ablation process and the laser was used at appropriate settings, char was not seen, regardless of the size/volume of the treated tissue.21 These results agree with an earlier study by Romano et al22 using Er:YAG lasers to cut cortical bone. These investigators observed a linear increase of ablation depth with the number of pulses. A greater number of pulses translates into more ablative energy in the area being irradiated per unit time. It was found that as long as adequate water spray was provided to the area, more bone was ablated with additional pulses (per unit time) without the char formation that would normally be an expected consequence of extra heat from the added pulses. It was also calculated that repetition rates beyond 20 Hz would not significantly increase the peripheral thermal damage to the bone. (Note: Hz [hertz] is the International System of Unit’s measurement for electromagnetic radiation per second. Ten Hz equals 10 laser pulses per second). These studies are germane since all commercially available FDA-approved Er:YAG dental lasers function from 7 to 30 Hz with a continuous water spray option.
In an attempt to quantify and illuminate the important thermal interactions of erbium lasers with calcified biologic tissues, it is important to review the inherent quantum mechanics and spectroscopy characteristics of the erbium laser/water interaction. In a study conducted by Shori et al23 describing the quantum mechanics of the water molecule under erbium irradiation, it was demonstrated that as water absorbs more of the incident energy of an Er:YAG laser and the temperature of the water increases, the length and strength of the oxygen-hydrogen bonds in the water molecule changes because of the large increase in kinetic energy. In addition, as this lengthening and weakening of the bonds occurs, the absorption peak for the water molecule shifts to wavelengths that are significantly shorter than 2.94 um. This negative shift in the absorption peak for water greatly diminishes the effectiveness of the beam to perform controlled thermal mechanical ablation on tissues.
The findings of Shori et al23 have important implications for how erbium lasers interact clinically with calcified biologic tissues. If more heat than is necessary to induce ablation is delivered to tissue, the negative absorption coefficient shift in water will be larger and more profound. This quantum, spectroscopic, and thermal reality associated with erbium lasers needs to be clearly understood by the clinician contemplating osseous surgery with an erbium laser. To prevent excess thermal deposition and a less effective thermal mechanical ablation, the clinician should keep a continuous water spray on the irradiated area to act as a heat sink and use the least amount of energy necessary to avoid the occurrence of the negative absorption shift.
 |
 |
| Figure 5. Er:YAG alveoloplasty of mandibular ridge prior to implant placement. Note heavy water spray on ablation area. | Figure 6. Continued alveoloplasty of mandibular ridge with Er:YAG laser prior to implant placement. |
 |
 |
| Figure 7. Creating a window in maxillary bone with Er:YAG laser apicoectomy procedure. Note heavy water spray on ablation area. | Figure 8. Complete lack of char and carbonization with free bleeding at apicoectomy site created with the Er:YAG laser. |
Recently, Sasaki et al24 analyzed the effects of bone removal by the Er:YAG laser under scanning electron microscopy and infrared spectroscopy. They concluded that the Er:YAG laser ablation of bone produced a groove with similar dimensions to that of a drilling bur. In addition, the chemical composition of the bone surface after Er:YAG ablation was much the same as that following bur drilling. Furthermore, the production of toxic substances was not observed following Er:YAG laser irradiation or conventional bur drilling of bone. Their conclusion was that the use of Er:YAG laser ablation may represent an alternative approach for oral and periodontal osseous surgery (Figures 5 through 8).
CONCLUSION
Reviewed in this article were (1) the literature pertaining to the potential use of the dental Er:YAG laser for osseous surgery and (2) an overview of current clinical use for soft tissue and tooth enamel applications. Presently in the United States, there is only one laser wavelength that is FDA-approved for intraoral osseous surgery—the Er:YSGG laser, which produces photons at 2.79 µm.25 Eversole and Rizoiu, describing the cutting of cortical rabbit tibia with this hydrokinetic Er,Cr:YSGG laser system, showed that when this laser system was used at 140 microseconds and 20 Hz, 24 hours post exposure photomicrographs of the wound cavities presented histology characteristic of a thermal coagulative effect, with a zone measuring 40 to 60 µm, similar to that of a dental bur.26 In this review of the literature, the data examining the photobiology of the Er:YAG laser supports its use in intraoral osseous surgery. As discussed in this review, if the criteria of rapid and char-free tissue ablation21 and excellent water absorption characteristics with precise bone cutting20 are considered, the Er:YAG laser should be considered safe for intraoral osseous surgery.
References
1. Einstein A. Zur Quantentheorie der Strahlung. Physiol Z. 1917;18:121-128.
2. Maiman TH. Stimulated optical radiation in ruby. Nature. 1960;6:493-494.
3. Hale GM, Querry MR. Optical constants of water in the 200 nm to 200 um wavelength region. Applied Optics. 1973;12:555-563.
4. Gerber BE, Knight M, Siebert WE, eds. Lasers in the Musculoskeletal System. New York, NY: Springer-Verlag; 2001:11-17.
5. Aoki A, Watanabe H, Ishikawa I. Er:YAG clinical experience in Japan: a review of scientific investigations. SPIE Proc. 1998;3248:40-45.
6. Lanigan SW. Lasers in Dermatology. London, England: Springer-Verlag; 2002:57-79.
7. Venugopalan V. Pulsed laser ablation of tissue: surface vaporization or thermal explosion? SPIE Proc. 1995;2391:184-189.
8. Walsh JT Jr, Flotte TJ, Deutsch TF. Er:YAG laser ablation of tissue: effect of pulse duration and tissue type on thermal damage. Lasers Surg Med. 1989;9:314-326.
9. Walsh JT Jr, Deutsch TF. Er:YAG laser ablation of tissue: measurement of ablation rates. Lasers Surg Med. 1989;9:327-337.
10. Neev J, Links JLS, Calderon N, et al. Thermo-optical skin conditioning: a new method for thermally modifying skin conditions. SPIE Proc. 2002;4609:94-106.
11. Niemz MH. Laser-Tissue Interactions: Fundamentals and Applications (Biological and Medical Physics). 2nd ed. Berlin, Germany: Springer-Verlag;2002:45-80.
12. Kesler G, Koren R, Kesler A, et al. Periodontal plastic surgery: thermal effect analysis using Erbium:YAG Kesler’s handpiece. Histochemical evaluation by Picrosirius red stain and polarization microscopy for collagen determination. SPIE Proc. 2000;3910:2-11.
13. Research, Science and Therapy Committee of the American Academy of Periodontology. Lasers in periodontics. J Periodontol. 2002;73:1231-1239.
14. Moshonov J, Stabholz A, Leopold Y, et al. Lasers in dentistry. Part B—Interaction with biological tissues and the effect on the soft tissues of the oral cavity, the hard tissues of the tooth and the dental pulp [in Hebrew]. Refuat Hapeh Vehashinayim. 2001;18(3-4):21-28,107-108.
15. Wigdor HA, Visuri SR, Walsh JT Jr. Effect of water on dental material ablation of the Er:YAG laser. SPIE Proc. 1994;2128:267-272.
16. Visuri SR, Walsh JT, Wigdor HA. Erbium laser ablation of hard tissue: modeling and control of the thermal load. SPIE Proc. 1994;2134A:130-133.
17. Freiberg RJ, Cozean CD. Pulsed erbium laser ablation of hard dental tissue: the effects of atomized water spray versus water surface film. SPIE Proc. 2002;4610:74-84.
18. Ando Y, Aoki A, Watanabe H, et al. Bactericidal effect of Er:YAG laser on periodontopathic bacteria. Lasers Surg Med. 1996;19:190-200.
19. Clayman L, Kuo P, eds. Lasers in Maxillofacial Surgery and Dentistry. New York, NY: Thieme Medical Pub; 1997:19-28.
20. Frenz M, Hausler R, Weber HP. Laser applications in middle ear surgery: advantages and possible side-effects. SPIE Proc. 2002;4609:295-302.
21. Truong MT, Majaron B, Pandoh NS, et al. Erbium:YAG laser contouring of the nasal dorsum: a preliminary investigation. SPIE Proc. 2001;4244:113-120.
22. Romano V. Bone microsurgery with IR-lasers: a comparative study of the thermal action at different wavelengths. SPIE Proc. 1994;2077:87-97.
23. Shori RK, Walston AA, Stafsudd OM, et al. Quantification and modeling of the dynamic changes in the absorption coefficient of water at __= 2.94 µm. IEEE Journal on Selected Topics in Quantum Electronics. 2001;7:959-970.
24. Sasaki KM, Aoki A, Ichinose S, et al. Scanning electron microscopy and Fourier transformed infrared spectroscopy analysis of bone removal using Er:YAG and CO2 lasers. J Periodontol. 2002;73:643-652.
25. Food and Drug Administration. 510k Summary of Safety and Effectiveness Information: Waterlase Millenium, hydrokinetic tissue cutting system. K013908
26. Eversole LR, Rizoiu I, Kimmel A. Osseous Repair Subsequent to Surgery With an Erbium Hydrokinetic Laser System, International Laser Congress, International Proceedings Division, Sept 25-28, Athens, Greece, 1996. pp 213-221.
Dr. Bornstein graduated from Tufts University School of Dental Medicine in 1992 and the Maimonides Medical Center General Practice Residency Program in Brooklyn, NY, in 1993. He practices general, implant, and laser dentistry in Natick, Mass, and operates the Metrowest Maxillofacial Imaging Center at the same location.
Disclosure: Dr. Bornstein is a consultant for OpusDent USA concerning matters of photobiology and laser tissue thermodynamics. He owns 2 combination Er:YAG/CO2 dual-wavelength lasers and 2 830-nm diode lasers, all purchased from Opusdent USA.
Dr. Lomke graduated from the University of Maryland Baltimore College of Dental Surgery in 1979 and from a US Public Health Service General Practice Residency in 1980. He practices general, laser, and aesthetic dentistry in Silver Spring, Md. He has achieved the level of educator status with the Academy of Laser Dentistry, with advanced proficiency in erbium and diode wavelengths.
Disclosure: Dr. Lomke is a clinical instructor for OpusDent USA. He owns a dual-wavelength Er:YAG/CO2 laser and a 830-nm diode laser, both purchased from OpusDent USA.