One of the most compelling trends in dentistry is the shift toward microdentistry, which is the practice of removing the least amount of tooth structure, bone, or tissue necessary to eliminate pathology, then replacing it (when applicable) as conservatively, comfortably, and aesthetically as possible. This paradigm shift in dentistry is moving dentists away from the practice of “wait-and-treat” dentistry to a significantly more proactive form of “diagnose-and-treat” dentistry. Today’s most advanced dentists must think in terms of “absence of disease as a model of health.” 1,2 Caries is an infectious disease resulting from Streptococcus mutans and Lactobacillus-two malicious pathogens that need to be treated thoroughly pathogenically and not as a mere excuse to put a hole in the patient’s tooth.3-5 In a landmark study, Weerheijm, et al,6 found cariogenic microorganisms in 53% of dentin samples cultured from sealed carious lesions, while soft dentin was present in all teeth studied. The key to minimally invasive microdentistry is prevention and early accurate caries diagnosis followed by micro-invasive treatment and placement of biomimetic restorations-that is, restorations using materials that most closely mimic natural tooth structure. For example, biomimetic materials such as glass ionomer and composite are used to replace dentin and enamel, respectively.
 |
 |
| Figure 1. Note shiny appearance of the peripheral rim of enamel as compared with the duller appearance of the remainder of the occlusal surface. | Figure 2. Note delamination of buccal and lingual walls from occlusal surface. |
DIAGNOSIS OF CARIOUS LESIONS IN MICRODENTISTRY
Accurate diagnosis requires a number of important items and steps, such as the following: (1) Consistent use of magnification and illumination using loupes and headlamps or a microscope. (2) An understanding of the caries process and the variability of fissure anatomy. (3) Quality radiography. Digitally enhanced radiographs aid in proper diagnosis. (4) Laser caries diagnosis (the DIAGNOdent, KaVo America). (5) Caries detection dye. Use of an explorer to detect occlusal decay has been consistently proven to be only about 25% accurate.7-9 In addition to the inaccuracy, clinical research conducted by Sturdevant has shown that forceful probing of the initial lesion can result in damage to the weakened porous enamel and result in accelerating the lesion.10 Radiographs have been proven to be even less accurate for early occlusal decay.11,12 Christensen has reported that “although the concept of ‘watching’ radiographically observable caries for a period has been standard practice, continuation of the concept for all patients is questionable.” 13 The DIAGNOdent, when used properly, has been shown to be about 90% accurate for occlusal decay.14 One note when using a system like the DIAGNOdent: once tooth structure has been altered with a laser, it’s fluorescence will cause a false positive reading for decay. Caries indicator dye will also cause a false-positive because a lased surface becomes porous and retains the dye.15
 |
 |
|
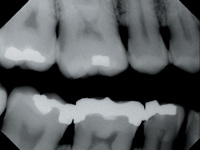
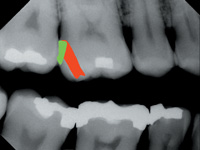
Figure 3. Note distal lesion on upper first molar |
Figure 4. Note how tunnel preparation indicated in red would result in considerably more loss of healthy tooth structure than a slot preparation, indicated in green. |
THE ERBIUM, CHROMIUM: YSGG LASER
Once decay or other pathologies are discovered, the Erbium, Chromium: YSGG (Er, Cr: YSGG) laser is an ideal instrument to perform safe, minimally invasive treatment. Using hydrokinetic energy, the laser allows the operator to all but eliminate the thermal damage, vibration, and microfractures of enamel associated with even the most sophisticated and advanced high-speed handpieces available today.16 Also, in many cases, local anesthesia and its possible side effects are eliminated because of the laser’s seeming analgesic and anesthetic effect on target tissue. The Er, Cr: YSGG is even effective on soft tissue as well, taking advantage of the unique nature of the Er, Cr: YSGG wavelength, which allows for no charring or damage to adjacent collateral tissue, which occurs with other laser wavelengths commonly used. Also, there is apparently faster healing and less postoperative discomfort for the patient.17 As with hard-tissue procedures, local anesthesia is often not necessary with soft-tissue surgeries. The same parameters and effects occur on bone as well.18
USING THE ER, CR: YSGG FOR CONSERVATIVE CLASS I-VI PREPARATIONS
The Er, Cr: YSGG is an ideal instrument for class I-VI cavity preparations. Once decay is identified, the laser can be used to remove occlusal tooth structure and mesial and distal interproxmial decay even in posterior teeth. Plus, the Er, Cr: YSGG allows for conservative preparation of worn incisal edges, subgingival class Vs and, to the delight of any dentist hoping to practice minimally invasive microdentistry, the Er, Cr: YSGG is an elegant tool for class II preparations.
 |
 |
| Figure 5. Contact point caries suitable for a tunnel preparation | Figure 6. Widespread rapid onset caries, more suitable for a slot preparation |
GUIDELINES FOR MINIMALLY INVASIVE LASER USE
Following these simple rules will help ensure the most conservative, long-lasting and comfortable treatment: (1) Use the smallest diameter tip that will accomplish the task efficiently. (2) Use the lowest possible power setting on hard or soft tissue that will achieve your goal in a time-efficient manner. (3) When using a tapered tip or an endo/perio tip, never exceed 2.5 watts. (4) Remove only the amount of tooth structure necessary to eliminate the decay. (5) Learn to focus and defocus the tip of the laser to achieve different effects, rather than constantly changing settings on the front panel. The fastest or most efficient cutting occurs when the laser tip is 1 to 1.5 mm from the target tissue surface-also known as the “active cutting zone.” Increasing the distance of the laser tip from the surface will lessen the effectiveness of the cut. Moving closer than 1 to 1.5 mm results in a muffling of the hydrokinetic effect; cutting will be curtailed, and discomfort may occur because of the transference of raw laser energy that hasn’t achieved its hydrokinetic association with the water spray. (6) The faster the operator moves the tip across the surface, the slower it cuts. (7) On soft tissue, the ideal effect is to end up with pink tissue postoperatively. Second best is white tissue and worst is charring-this means excessive heat and visible tissue trauma. To avoid these effects, use the lowest setting possible and short, quick brushing strokes to excise soft tissue. The result is faster healing and less postoperative discomfort.
CLASS II COMPLETED USING MICRODENTISTRY TECHNIQUES
The class II procedure lends itself to closer examination, since it is one of the toughest and most involved restorative procedures a dentist can perform. It is also the type of case that can easily result in an excessive amount of tooth structure being removed. During a class II, it is extremely important to the long-term health of the dentition that we be as conservative as possible in preparing and restoring class II lesions. Especially important is the preservation of the peripheral rim of enamel, as described by Rainey and Milicich.19 The marginal ridge is a part of a distinct rim of enamel around the occlusal surface that is one of the main stress distribution structures in a tooth. The demarcation between this and the occlusal enamel can be clearly identified (Figure 1). Once the stress distribution system of the tooth is disturbed by a cavity, this demarcation zone becomes clinically evident. We often see what appears to be delamination of the walls of the tooth from the occlusal surface, as shown in Figure 2. To maintain the integrity of the tooth whenever possible, the operator should complete a tunnel preparation, or slot preparation, or when access permits, treat the lesion as though it were a class III. Certain factors must be considered when deciding which type of preparation to use. First, where is the caries in relation to tunnel access? Note Figures 3 and 4. In this instance, the tunnel preparation option would volumetrically involve considerably more loss of tooth structure than a slot preparation, and so the latter would be less invasive.5 Second, in high caries risk patients, slot preparations or class II type preparations may be a better choice than a tunnel preparation. Rapid onset caries with early cavitation is more suitable for slot preparations, while slow onset noncavitated contact point caries is ideal for tunnel preparations. In high caries risk patients, the interproximal demineralization often extends well into the embrasures, and a tunnel preparation will not completely isolate the underlying dentin from the microporous enamel.20
CONCLUSION
With a dramatic paradigm shift in treatment methodologies occurring in the dental profession, it is extremely important that dentists understand the concepts, techniques, and tools available to practice microdentistry. The benefits to the patient are staggering: significant preservation of their healthy dentition and the minimization of rampant tooth failure and loss as caused by standard treatment protocols. There are organizations that educate dentists about microdentistry, including the World Congress of Microdentistry, which meets annually (visit wcmicrodentistry.com for information on meetings and seminars). Take whatever opportunities you can to educate yourself on this exciting new trend of microdentistry. The health and integrity of every tooth you treat can be improved with these exciting new techniques and instruments.
Acknowledgment All figures courtesy of Dr. Greame Milicich of New Zealand.
References
Dr. Rosenberg is a pioneer and innovator in the use of dental lasers, micro-air abrasion, and other high-tech dental instruments and applications. He is a founder, diplomat, and president of the World Congress of Microdentistry, was Clinician of the Year, and recipient of the Distinguished Service award. He is a founder, master, and past president of the Academy of Laser Dentistry and recipient of the academy’s Distinguished Service Award. He is a fellow of the International Society of Laser Dentistry, the American Society of Laser Medicine and Surgery, the International College of Craniomandibular Orthopedics, the Academy of General Dentistry, and the Academy of Stress and Chronic Disease. Dr. Rosenberg is an active member of The American Academy of Cosmetic Dentistry, the American Equilibration Society, a founder and member of the board of directors of the World Clinical Laser Institute, and a member of many other organizations. While maintaining a busy private practice emphasizing cosmetic and advanced dentistry, he serves as an attending doctor at Johns Hopkins Hospital. Dr. Rosenberg can be reached at (301) 776-3300 or at srosenberg8@comcast.net.








