Randolph R. Resnik, DMD, MDS, shares some valuable thoughts with Dentistry Today’s implant editor, Michael Tischler, DDS, based on his experience as an implantologist.
What role do you think general dentists will play in implantology in the future?
Dr. Resnik: In my opinion, general dental practitioners (GPs) are going to play an even more significant role in the future of implant dentistry. Statistics show that the number of GPs in the United States who are placing dental implants continues to increase every year, but it remains well behind the number of dentists placing implants worldwide. Only about 15% of GPs in the United States place implants, while almost 90% of GPs worldwide place implants. With the average growth rate of dental implants at approximately 5% to 8% per year, I believe that more GPs will get involved with the surgical placement of implants. GPs are in the perfect position to build an implant practice as they are usually the first line in evaluating patients with advanced decay, fractured teeth, failing prostheses, and masticatory deficiencies.
 |
 |
 |
| Figure 1. A congenitally missing lateral incisor implant case: (a) the preoperative view, (b) final postoperative clinical image, and (c) final post-op radiograph. |
Do you believe GPs should be placing dental implants?
Dr. Resnik: Most definitely. First, every GP has the skill set to be placing dental implants. Many GPs believe dental implants are very difficult to learn and that they require a great deal of surgical expertise. This is completely false. In most cases, extracting a tooth or completing a root canal is far more difficult than placing an implant. The difficulty involves dentists learning ideal patient and case selection, especially early on in their learning curves. This is why I place so much emphasis on treatment planning at the Misch Implant Institute, as I believe this directly correlates with a successful and profitable private implant practice. If a GP learns the difference between an ideal and a non-ideal case, it can take his or her practice to the next level. This is one reason why my textbook, Avoiding Complications in Oral Implantology (Elsevier Publishing), has been so successful: It is a comprehensive review of surgical and prosthetic complications, with an emphasis on their etiology, management, and prevention.
 |
 |
 |
 |
| Figure 2. A mandibular posterior implant case: (a) a failing mandibular posterior prosthesis (teeth Nos. 17 to 20), (b) implant placement, (c) the final prosthetic abutments, and (d) the final posterior implant prosthesis. |
How could more GPs become involved in placing dental implants?
Dr. Resnik: First, the general dentist must obtain adequate education in dental implants. Because most dental students receive very little exposure while in school with respect to dental implants, most can learn what they need to know to get started very quickly through dental education seminars. At the Misch Institute, our studies show almost 98% of graduates are placing dental implants, along with an average increase of 22% in their yearly incomes. Dentists just need to realize that they do not have to treat every case. That is why our curriculum is set up so that the attendees can learn specific procedures that are straightforward and predictable. Therefore, developing a strong foundation with accepted principles allows the clinician to treat patients successfully and predictably.
Isn’t it expensive to get started in placing dental implants?
Dr. Resnik: In the past, I would have definitely agreed with that statement since everything involved with dental implants was expensive (eg, implants, prosthetic parts, lab fees, and education). However, and fortunately, times have changed! Since our partnership with Glidewell Laboratories, our Misch attendees can get involved in implant dentistry with minimal initial investment. Historically, the investment to get started was very costly. Glidewell has allowed our graduates to obtain everything they need to start placing implants (an implant motor, a handpiece, the Hahn Tapered Implant System (Glidewell Laboratories), a surgical kit, and a prosthetic kit) for an investment that is far less than what implant motors themselves have cost in the past. In addition, Glidewell offers a discount on the laboratory work for cases where the Hahn Tapered Implant System is used. In my opinion, there has never been a better time to get started in the field!
 |
 |
 |
 |
 |
| Figure 3. A mandibular implant-supported overdenture: (a and b) five implants inserted between the foramen, (c) a splinted bar, (d) a prosthesis with attachments, and (e) the final prosthesis. |
Where do doctors find the best patients to get started on this journey?
Dr. Resnik: General dentists see potential dental implant patients every day in their offices. Dentists need to learn to explain the benefits of dental implants to their patients, along with the disadvantages of any alternative conventional treatment plans. For example, when a single tooth is lost, there exist many benefits to placing an implant instead of preparing the adjacent teeth for a fixed partial denture. Studies show that an abutment tooth prepared for a crown has an approximate 14% chance of developing irreversible pulpitis, which would necessitate endodontic therapy. This often leads to increased costs for the patient or a loss of patient confidence in the doctor. When evaluating 10-year survival rates, a greater than 25% improved implant prosthesis survival rate is seen when compared to a fixed partial denture supported by natural teeth. Almost all dental implant survival and success studies report a greater than 95% success rate for dental implants, which is much higher than any other type of implant that is placed in the body.
 |
 |
| Figure 4. An implant placement and sinus graft case: (a) the pre-op radiograph, and (b) the final image showing the implant and sinus augmentation. |
What has changed the most in implant dentistry from when you first started on your journey 30 years ago?
Dr. Resnik: The most significant change in implant dentistry is the ability to rehabilitate very compromised implant sites that, in the past, were thought to be impossible. In the early days of implant dentistry, many patients were simply deemed not suitable as candidates for dental implants. However, with the new technologies, simplified procedures, and predictable techniques that are available to restore patients back to dental health, the landscape for implants has changed dramatically.
Bone grafting procedures are now available that are less invasive and less complicated. Well-documented socket grafting techniques allow the clinician to maintain and possibly increase the amount of bone available after tooth extraction. Guided-bone regeneration procedures have been technologically enhanced with predictable bone substitutes and bone growth factors. This allows for accelerated and predictable healing. In addition, the integration of cone beam computed tomography (CBCT) and guided surgery into both general and specialist dental practices has really changed how patients are surgically and prosthetically planned and treated.
 |
 |
 |
 |
| Figure 5. An immediate load case: (a) the pre-op radiograph, (b) extraction and maxillary implant placement, (c) extraction and mandibular implant placement, and (d) immediate insertion of the maxillary and mandibular fixed prostheses. |
How can the use of CBCT help GPs with dental implant treatment?
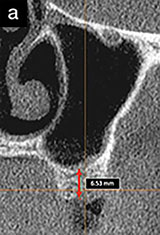
Dr. Resnik: The use of CBCT has allowed clinicians to treat patients with dental implants more predictably. First, CBCT allows the clinician to determine the exact available bone quantity and quality. This makes the treatment planning phase much easier and more accurate than in the past. Clinicians will know the exact bone morphology prior to the surgery. Because of this technology, the need for bone augmentation may be ascertained, and the exact size implant may be determined, all in advance. Also, with the use of guided surgery, implants are able to be positioned precisely according to the intended final prostheses. This leads to fewer complications and to more predictable aesthetic and functional results. With fully guided surgery, implants can now be inserted directly through the surgical guide, which is based on 3-D, interactive treatment planning prior to surgery.
Thanks for carving time out of your busy schedule to do this interview for our Dentistry Today readers, Randy! Thanks especially for your expertise and perspectives on how interested GPs can get started placing implants in their own practices.
Dr. Resnik is a leading clinician, educator, researcher, and author in the field of prosthodontics and has a fellowship degree in oral implantology. Dr. Resnik has received a specialty degree in prosthodontics and oral implantology from the University of Pittsburgh, along with a Master’s degree in oral implantology/radiology. He is currently the chief of staff and surgical director of the Misch Implant Institute. He also holds faculty positions at the University of Pittsburgh (graduate prosthodontics), Temple University (graduate periodontics), and Allegheny General Hospital in Pittsburgh (oral and maxillofacial surgery). Along with his passion for lecturing and education, Dr. Resnik is also an accomplished author, having published numerous research articles and textbooks across his career. His recent textbook, Avoiding Complications in Oral Implantology, is a best seller. He has also been a contributing author to all 3 editions of Contemporary Implant Dentistry and 2 editions of Dental Implant Prosthetics. He can be reached at resnikdmd@gmail.com.
Disclosure: Dr. Resnik reports no disclosures.
Related Articles
The Dreaded Loose Abutment Screw: Etiology, Management, and Prevention
Bone Grafting for Dental Implant Placement



