INTRODUCTION
Since the advent of original resin-based composites developed in the 1960s, the ability to match adjacent tooth structure has been of utmost importance. One of the greatest attributes of composites over amalgam is that they approximate the natural color of the human dentition. Initially, our profession was simply happy to have a material that did not start out as a silver filling (that eventually turned black) while corroding and expanding to place pressure on the preparation walls.
There were a number of hurdles to overcome with resin-based restoratives, including issues related to polymerization shrinkage; excessive heat from exothermic curing; poor flexural, tensile, and compressive strengths; and poor wear resistance. Each of these critical factors has been overcome with the incredible advancements in composite resin material science over the past 30 years. With an increasingly high emphasis on aesthetics, the desire to exactly match the surrounding enamel at the cavosurface margin has always been one of the most challenging and important tasks in achieving aesthetic success. To accomplish appropriate color matching, most dentists are required to keep a large inventory of composite systems with an extensive range of shades. There are a number of disadvantages to this restorative model:
- The monetary cost of carrying multiple systems is a financial burden with poor returns.
- Multiple composite systems with multiple shades and dispensing methods take up significant physical space.
- A variety of adhesives may be required to accommodate the above composite systems.
- There is a high likelihood that many infrequently used or obscure shades will expire before the materials are ever even taken out of their packages.
- The use of many of these technique-sensitive materials requires training and an advanced skill set for placement, often involving a number of shades and specific layering procedures.
- All this effort requires extra time for both the patient and the restorative team.
A Single-Shade Composite Restorative Solution
When I first heard that a new, genuinely universal composite was being introduced, the famous saying from President Ronald Reagan came immediately to mind: “There you go again!” He would say it as a way of disarming his opponent, implying that they spoke with hyperbole or even falsehood. Over more than 3 decades of practice, I’ve read of the single-shade composite claim a number of times, without any of them ever truly achieving the goal. Hope was always followed by disappointment. So, it was with a healthy degree of skepticism that we beta tested OMNICHROMA (Tokuyama Dental America) composite resin restorative material. However, we were pleasantly surprised!
 |
| Figure 1. OMNICHROMA (Tokuyama Dental America) is available for delivery in both syringes and individual compules. |
To begin with, the physics of composite resin and color were completely rethought. All other current composite materials rely on the chemical color of the resin to emulate certain shades of human teeth. Traditional composites are limited in their ability to shade match, meaning the doctor must pick a shade that is the same as the substrate being restored. For example, a tooth with VITA B1 enamel will require a B1 composite, while a C4 tooth will clearly not match that same B1 material. And teeth, of course, do not represent a single shade! A simple Class I cavity preparation may have an A4 cavity prep floor, dentin walls that appear as D3, and enamel that is B2 at the proximal ends but B1 near the cuspal inclines. Proper use of the current chemical color-based composites may require as many as 4 or 5 different shades to achieve a true match.
OMNICHROMA (Figure 1) utilizes Smart Chromatic Technology to leverage structural color as a way of matching the surrounding substrate. It relies on the material transmitting the color of adjacent tooth structure to provide a restoration that matches. This technology is not the same as using a translucent material that allows color to reflect through it. Structural color can be best appreciated when looking at a soap bubble, or the grooves on a compact disc, and seeing the rainbow reflection off of the surface. This myriad of colors is the result of microscopic structures physically interacting with light.
So, how is the structural color of Smart Chromatic Technology different than ordinary chemical color in composite restorative chemistry? Starting with the size and shape of the filled resin particles, OMNICHROMA utilizes supra-nano spherical SiO2-ZrO2 particles that are uniformly 260 nm in size. When compared on SEM with all other composites on the market, 2 obvious characteristics jump out—the consistent shape and the small particle size (Figures 2 and 3).
This unique filler size and shape allows for the natural color of the surrounding tooth to reflect through and with the OMNICHROMA material, which, by design, is created to be most effective in the red-to-yellow range of the spectrum. Human teeth have a natural chroma in the red-to-yellow range.
Let’s now look at a clinical example using this innovative composite resin.
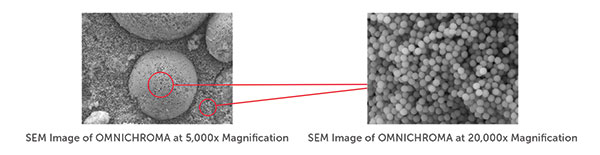 |
| Figure 2. SEM image comparison of OMNICHROMA and other typical composite resins. |
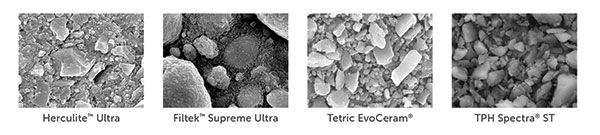 |
| Figure 3. Note the irregular shape and size of other composite fillers. |
CASE REPORT
Diagnosis and Treatment Planning
A 60-year-old male patient with dental anxiety presented with a number of restorative issues (Figures 4 and 5). A recent root canal treatment had been done on a zirconia-crowned No. 4 with the pulp chamber sealed using an orange core material, and it was in need of an access-fill restoration. A loose screw-retained zirconia implant crown No. 5 in need of having its abutment screw replaced and access hole restored was noted. And, finally, a buccal Class V composite restoration on tooth No. 20 with recurrent decay was in need of replacement.
Clinical Protocol
The following is a description of the clinical steps taken to maximize efficiency and reduce chair time for our anxious patient.
1. Local anesthetic was administered for the restoration of tooth No. 20.
2. During the latent period, while the anesthetic was taking effect on No. 20, the access hole on the screw-retained implant crown No. 5 was opened, and the old abutment screw was removed. The implant crown and implant table were evaluated and determined to be healthy, and a new abutment screw was placed and torqued to the proper value. Yellow Teflon tape, impregnated with silver nitrate to reduce bacterial presence, was placed in the implant access chamber. The occlusion was evaluated using Madame Butterfly Blue Silk (Pankey Institute) articulation ribbon. A periapical radiograph was taken to determine a full seating of the screw-retained implant crown. A small cotton pledget was placed over the Teflon tape for step 3 (below) and then removed for step 4 (below).
 |
 |
| Figure 4. Preoperative photo of the access openings of teeth Nos. 4 and 5. | Figure 5. Pre-op photo of tooth No. 20 with a failing Class V buccal composite with recurrent decay. |
 |
 |
| Figure 6. OMNICHROMA was placed in the endodontic access opening of prepared tooth No. 4. | Figure 7. OMNICHROMA was placed in the implant access channel of tooth No. 5. Note that both composites have not been polymerized and the significant color difference with the adjacent crown structure. |
 |
 |
| Figure 8. Light cure of both teeth Nos. 4 and 5. | Figure 9. Final restorations of teeth Nos. 4 and 5. |
 |
 |
| Figure 10. Removal of failing old composite restoration on tooth No. 20. | Figure 11. Recurrent decay was observed at the gingival level of tooth No. 20. |
 |
 |
| Figure 12. OMNICHROMA placement in the prepared Class V cavity on the buccal wall of tooth No. 20. | Figure 13. Immediate postoperative photo of the final restoration of tooth No. 20. |
 |
| Figure 14. Note the color difference between the incrementally placed and cured OMNICHROMA material adjacent to the uncured material in this restoration. |
3. Both the zirconia implant crown No. 5 and the recently endodontically treated tooth No. 4 (done through an existing zirconia crown) were micro-air abraded (PrepStart [Zest Dental Solutions]) with 27.5 µm AlO2 at 40 psi to clean the ceramic surfaces. A 9% hydrofluoric acid (HF) porcelain etchant (Porcelain Etch [Ultradent Products]) was placed and allowed to set for 30 seconds to improve micromechanical retention. The HF etchant was thoroughly rinsed away, being careful to avoid contact with oral tissues. A 35% phosphoric acid gel (Ultra-Etch [Ultradent Products]) was then utilized for 10 seconds to remove any remaining salts. After rinsing, to remove phospholipids, Ivoclean (Ivoclar Vivadent) was placed, allowed to set for 20 seconds, and then thoroughly rinsed away. The access openings were rinsed and dried. Finally, a 2-part silane system (Bis-Silane [BISCO Dental Products]) was applied to maximize bond strength. These 5 steps take less than 2 minutes and ensure that a long-term, impenetrable seal of the composite material to the ceramic is achieved.
 |
| Figure 15. OMNICHROMA BLOCKER (Tokuyama Dental America) was used to provide proper substructure for the restorative material. |
4. Both access openings were treated with an eighth-generation bonding agent (Tokuyama Universal Bond [Tokuyama Dental America]) used due to its very high and reliable adhesive strength and the time it saves because of its simple placement technique. Tokuyama Universal Bond is a simple system: Mix a drop of bond A and B, place it on the prepared surface, air dry for a total of 10 seconds (5 seconds weak air, 5 seconds mild air), and proceed to composite placement. No agitation or light curing is necessary, allowing for worry-free polymerization in areas a curing light can’t reach while bonding to any substrate.
5. Both access holes were bulk filled with the universal one-shade OMNICHROMA composite to a depth of 3.0 mm (curing depth varies with curing light intensity). The composite was then contoured and light cured (VALO LED [Ultradent Products]) for 10 seconds at the Xtra Power setting (3,200 mW/cm2) (Figures 6 to 8).
6. The occlusion was evaluated and adjusted. Then both crowns were polished back to a high luster (CeraGlaze [Kavo Kerr]). In the 14 minutes spent to complete steps 1 through 6, the patient achieved profound anesthesia for decay removal on tooth No. 20 (Figure 9).
7. The original 10-year-old composite material was removed from the buccal aspect of tooth No. 20, with recurrent decay noted on both the mesial and cervical aspects of the preparation. Careful slow-speed rotary excavation allowed for no hard- or soft-tissue damage. A Zekrya Gingival protector (DMG America) was used to protect the sulcus during micro-air abrasion (PrepStart). A 35% phosphoric acid (Ultra-Etch) was applied to the full preparation for 30 seconds and copiously rinsed with water. MicroPrime G (Zest Dental Solutions) was placed, followed by light air drying (Figures 10 and 11).
8. The restoration of tooth No. 20 was accomplished by first placing Tokuyama Universal Bond, followed by the placement of OMNICHROMA composite in 2.0-mm increments. Each 2.0-mm increment was light cured with the VALO LED light for 10 seconds at high power (1,400 mW/cm2). The excellent sculptability of this composite material enabled a minimal need for post-cure contouring and adjustment. Simple polishing was accomplished (Enhance PoGo Polishing System [Dentsply Sirona]) with no need for the use of carbide finishing burs (Figures 12 and 13).
DISCUSSION
Over the past few decades, claims by manufacturers to have developed a universal, single-shade composite have fallen short of expectations. Smart Chromatic Technology has truly revolutionized composite restorative materials for cosmetic dentistry. The unique use of structural color to mimic adjacent tooth shades has provided numerous benefits to our profession and patient population. OMNICHROMA is easy to use and works with almost any shade while reducing inventory, cost, decision making, and time.
As with any material, there is a learning curve; however, it is minimal and easy to master. The first startling clinical observation will be the significant color difference between the uncured and final restorations. It takes a small leap of faith to know that the white-opaque uncured material will match the bordering structures after polymerization. The composite, once cured, does blend with its surroundings, unlike all other materials that rely on chemical colors for shade matching (Figure 14).
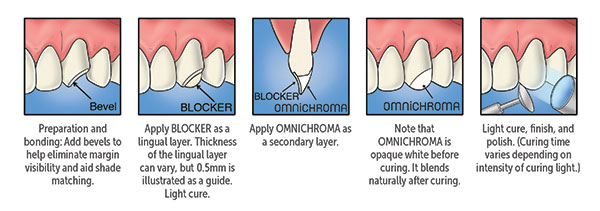
A second part of the learning curve is the use of OMNICHROMA BLOCKER (Tokuyama Dental America), a supplementary product that is necessary if no natural tooth structure matrix exists for the structural color to mimic. A full Class IV fracture can be restored utilizing a thin shelf of OMNICHROMA BLOCKER on the palatal surface (Figure 14), followed by a layer of OMNICHROMA. I have also found the blocking agent to be useful when filling endodontic access holes with dark pulp chamber floors or through porcelain-fused-to-metal crowns. Oftentimes, a multi-step opaquing process is necessary to blend the composite with the crown and not end up with a “manhole cover.” A small increment of OMNICHROMA BLOCKER, followed by a layer of OMNICHROMA, will result in a seamless repair. If the core material is lighter (or even orange, as seen in tooth No. 4), OMNICHROMA BLOCKER is not necessary (Figure 15).
CLOSING COMMENTS
The concept of structural color over chemical color restorative material is a proven technology that will simplify shade matching and revolutionize cosmetic dentistry. The introduction of this new single-shade, universal composite restorative material is a giant leap forward by providing excellent shade matching that requires minimal investment in time and by eliminating the need for keeping and maintaining an extensive inventory of differently shaded composites.
Dr. Gray is a 1986 graduate of the Georgetown University School of Dentistry. He is a Master and LLSR in The AGD and a Fellow in the International Congress of Oral Implantologists, International College of Dentists, and Academy of Dentistry International. He is an instructor at the LD Pankey Institute and at 9 universities. Dr. Gray has spoken on new dental technologies in more than 200 US cities and 10 countries since 1994. Dentistry Today has honored Dr. Gray as one of its Leaders in Continuing Education. Dr. Gray is an Invisalign Premier Provider and maintains a full-time, fee-for-service private practice in Washington, DC. He can be reached at bg@smiledc.com.
Disclosure: Dr. Gray is an unpaid consultant for Tokuyama Dental America.
Related Articles
Accelerated Orthodontics for the General Practitioner
Evolution and Revolution: Groundbreaking Changes in Composite Dentistry
Direct Composites: Shade-Matching Challenges











