INTRODUCTION
Traumatic ulcerative granuloma with stromal eosinophilia (TUGSE) is a relatively rare, benign granulomatous ulcerative oral mucosal lesion. TUGSE occurs more commonly among women compared to men. The prototypical appearance is that of a slow-healing ulcer with an elevated border, which is a similar clinical appearance to oral squamous cell carcinoma (OSCC). Therefore, a biopsy procedure is necessary to rule out (or rule in) OSCC. The condition is known to persist from one week to one year before resolution. The lesion tends to heal in a relatively quick fashion after a biopsy procedure. The etiology of TUGSE is unknown; however, trauma is believed to initiate the process. Recurrence is unusual.1-6
The most common location of TUGSE is the tongue. TUGSE lesions of the tongue are noted for occurring between 46% and 78% of the time. The incidence of occurrence on the floor of the mouth is between 3% and 7%. The sites for TUGSE that are less common are the retro molar area, gingiva, alveolar mucosa, lip, labial frenum, and palate. The buccal mucosa and vestibular mucosa sites are more common compared to the floor of the mouth but less common when compared to the tongue.1-4 el-Mofty et al7 reported 38 cases of TUGSE and noted 16 lesions of the tongue and 10 lesions of the buccal mucosa but reported no lesions of the floor of the mouth.
In 1890, Fede8 named the condition Riga-Fede’s disease and further described the histology. At the time, Riga-Fede’s disease was considered to be a pediatric condition. In 1983, Elzay9 utilized the term TUGSE to describe this lesion. When this condition occurs in the very young, it has been termed Riga-Fede disease. Other TUGSE lesion names include sublingual granuloma, traumatic granuloma, eosinophilic granuloma, and ulcerative eosinophilic granuloma.10,11
Here, we report on a singular case of TUGSE in a 28-year-old male patient with a long-term history of recurrent aphthous stomatitis/ulcers (RAS/RAUs) minor with the lesion occurring on the floor of the mouth.
CASE REPORT
The 28-year-old male patient presented to his general dentist in early September 2021 for a routine dental appointment. His chief complaint was a painful floor-of-the-mouth lesion. The patient described the pain as “sore.” The patient reported that the lesion first began 2 months prior and was somewhat responsive to topical steroid and local anesthetic therapeutics (dexamethasone elixir and 2% viscous lidocaine). The patient had assumed that the sore lesion on the floor of the mouth was another of his ongoing RAUs. The white lesion was approximately 2 cm in diameter and was noted for indurated, rolled borders (Figure 1). The patient was referred to an oral and maxillofacial surgeon to have a biopsy procedure within 2 weeks.

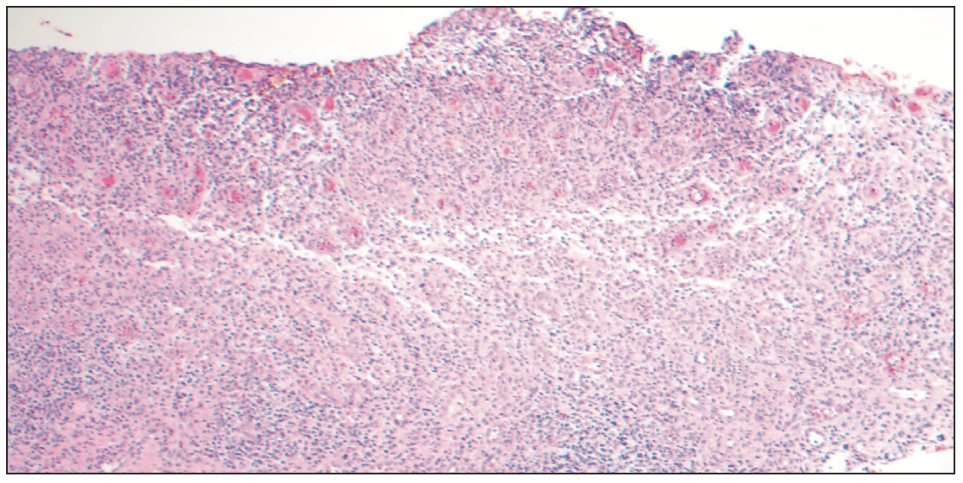
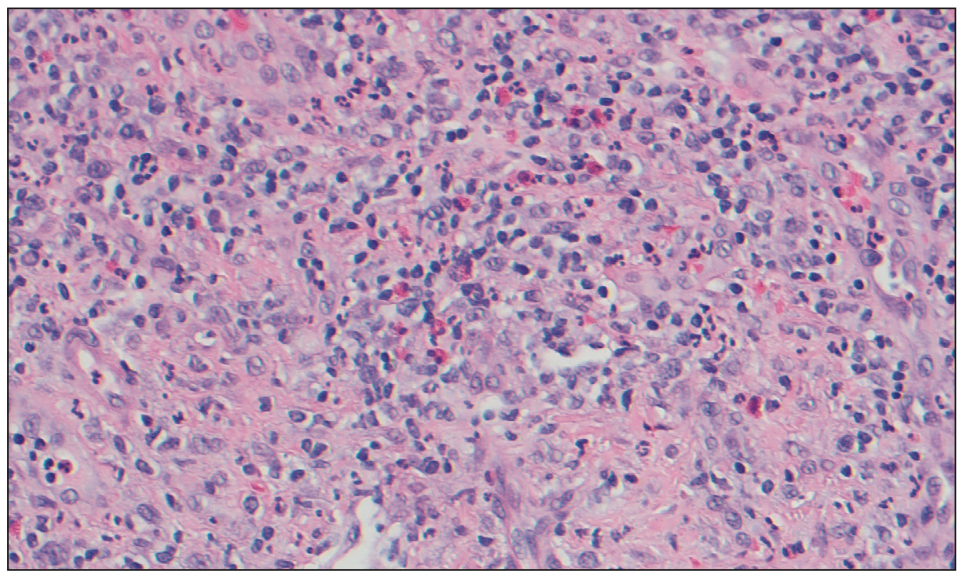
The biopsy report noted a large zone of surface ulceration consisting of a thin fibrinopurulent membrane. Also, there was a dense lymphohistiocytic and mononuclear cell chronic inflammatory infiltrate with numerous eosinophils extending into the fibrous connective tissue below the ulcer (Figures 2 and 3). There was no evidence of any malignant or neoplastic processes. The histopathologic diagnosis was TUGSE, a specific category of chronic oral ulcer that typically resolves following a biopsy procedure. True to form, the floor-of-the-mouth lesion resolved within 2 weeks of the biopsy.
The patient’s history of recurrent aphthous stomatitis/ulcers began in 2009. He was referred by an allergy and immunology physician and later to an oral medicine clinician in 2011. The lesions were typical target lesions (a white center with a red periphery) and were 1 cm or less in diameter, determining a diagnosis of minor RAS/RAU. The flares responded to topical dexamethasone elixir therapy and topical 2% viscous lidocaine solution. However, after one lesion completely resolved, another RAS/RAU lesion would occur in the not-too-distant future in a different oral mucosal location.
DISCUSSION
Benitez et al11 reported a histologic appearance characterized by a vague granulomatous appearance and, at times, a jigsaw-like appearance with a diffuse polymorphic inflammatory infiltrate of histiocytes, predominantly activated T-lymphocytes, and eosinophils. They also noted that the lesion tends to extend into the submucosa, deeper muscle fibers, and salivary glands.
In another presented case, Ficarra et al12 noted a dense cell infiltrate composed of eosinophils, lymphocytes, and large mononuclear cells. Furthermore, they reported that the infiltrate was mainly CD3+, CD4+, CD8=T-cells, and CD1a+dendritic cells. They noted that approximately 70% of the T-cells expressed CD30 (Ki-1) antigens and, therefore, a possible association with lympho-proliferative disorder. However, it is important to note that this case was rather unique in that the patient had had multiple reoccurrences of TUGSE.
There doesn’t appear to be any connection noted in the literature between the 2 conditions of TUGSE and RAS/RAU. It is certainly possible that an RAS/RAU lesion was a source of trauma to the floor of the mouth in this case. The patient had a long-term history of RAS/RAU flares, and it was natural for the patient to treat the floor-of-the-mouth sore lesions with topical steroid and local anesthetic topical therapeutics.13 With respect to the patient presented, the natural history, clinical appearance, and histopathology established the diagnosis of the floor of the mouth lesion as TUGSE. The 2-month duration established that the lesion was chronic, and the resolution within 2 weeks after the biopsy procedure was consistent with the expected natural history of TUGSE.5,6,10,11
It is established that TUGSE is a chronic ulcerative condition. The differential diagnoses include such diagnostic entities as traumatic ulcers, OSCC, CD30 lymphoproliferative disorder, syphilis, Epstein-Barr virus mucocutaneous ulcers, and RAS/RAUs. Indeed, the appearance of TUGSE tends to mimic OSCC, which emphasizes the necessity of biopsy procedures. The histopathologic picture is that of a characteristic eosinophilic granulomatous infiltrate.6,11
In conclusion, we have presented a case of TUGSE, which is a rare condition within the floor of the mouth, a relatively uncommon location for TUGSE. It is important for clinicians to have an appreciation with respect for the diagnosis, clinical appearance, natural history, and treatment of this lesion.
REFERENCES
1. Shen WR, Chang JY, Wu YC, et al. Oral traumatic ulcerative granuloma with stromal eosinophilia: A clinicopathological study of 34 cases. J Formos Med Assoc. 2015;114(9):881–5. doi:10.1016/j.jfma.2013.09.012
2. Salisbury CL, Budnick SD, Li S. T-cell receptor gene rearrangement and CD30 immunoreactivity in traumatic ulcerative granuloma with stromal eosinophilia of the oral cavity. Am J Clin Pathol. 2009;132(5):722–7. doi:10.1309/AJCPX3S5MSOVVLOP
3. Fonseca FP, de Andrade BA, Coletta RD, et al. Clinicopathological and immunohistochemical analysis of 19 cases of oral eosinophilic ulcers. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115(4):532–40. doi:10.1016/j.oooo.2012.11.007
4. Elzay RP. Traumatic ulcerative granuloma with stromal eosinophilia (Riga-Fede’s disease and traumatic eosinophilic granuloma). Oral Surg Oral Med Oral Pathol. 1983;55(5):497-506. doi:10.1016/0030-4220(83)90236-0
5. Sugaya N, Martignago F, Pinto D, et al. Recurrent oral eosinophilic ulcers of the oral mucosa. A case report. Open Dent J. 2018;12:19-23. doi:10.2174/1874210601812010019
6. Lakkam BD, Astekar M, Alam S, et al. Traumatic ulcerative granuloma with stromal eosinophilia: A puzzle. J Oral Maxillofac Pathol. 2021;25(Suppl 1):S42-S45. doi:10.4103/jomfp.JOMFP_321_20
7. el-Mofty SK, Swanson PE, Wick MR, et al. Eosinophilic ulcer of the oral mucosa. Report of 38 new cases with immunohistochemical observations. Oral Surg Oral Med Oral Pathol. 1993;75(6):716–22. doi:10.1016/0030-4220(93)90429-8
8. Fede F. Della produzione sottolinguale, o malattia del Riga: Atto Congresso Italiano di Pediatria. [On sublingual production, or Riga disease: Act of the Italian Pediatric Congress.] Atto Congresso Italiano di Pediatria. 1890;251-260. Italian.
9. Elzay RP. Traumatic ulcerative granuloma with stromal eosinophilia (Riga-Fede’s disease and traumatic eosinophilic granuloma). Oral Surg Oral Med Oral Pathol. 1983;55(5):497-506. doi:10.1016/0030-4220(83)90236-0
10. Sharma B, Koshy G, Kapoor S. Traumatic ulcerative granuloma with stromal eosinophila: a case report and review of pathogenesis. J Clin Diagn Res. 2016;10(10):ZD07-ZD09. doi:10.7860/JCDR/2016/22265.8657
11. Benitez B, Mulli J, Tzankov A, et al. Traumatic ulcerative granuloma with stromal eosinophilia – clinical case report, literature review, and differential diagnosis. World J Surg Oncol. 2019;17:184.
12. Ficarra G, Prignano F, Romagnoli P. Traumatic eosinophilic granuloma of the oral mucosa: a CD30+(Ki-1) lymphoproliferative disorder? Oral Oncol. 1997;33(5):375–9. doi:10.1016/s1368-8375(97)00014-6
13. Siegel MA. Chapter 16: Recurrent aphthous stomatitis. In: Siegel MA, Sollecito TP, Stoopler ET, eds. Clinician’s Guide to Treatment of Common Oral Lesions. 8th ed. American Academy Oral Medicine; 2017:26-28.
ABOUT THE AUTHORS
Dr. Brown is professor emeritus of the Howard University College of Dentistry, Department of Comprehensive Care, in the Division of Oral Diagnosis & Radiology, and a clinical associate professor in the Department of Otolaryngology at the Georgetown University Medical Center in Washington, DC. He can be reached at rbrown@howard.edu.
Dr. Castle earned his DDS degree from the Creighton University School of Dentistry and his certificate in oral and maxillofacial pathology from the Naval Dental School. Dr. Castle is a Fellow of the American Academy of Oral and Maxillofacial Pathology and a Diplomate of the American Board of Oral and Maxillofacial Pathology. He currently practices in the Department of Dermatology, Division of Oral and Maxillofacial Pathology, at Johns Hopkins Hospital. He can be reached at jcastl18@jhmi.edu.
Dr. Cherry-Peppers is an associate professor at the Howard University College of Dentistry, Department of Comprehensive Care, in the Division of Oral Diagnosis & Radiology in Washington, DC. She can be reached at gail.cherrypeppers@howard.edu.
Dr. McIntosh is an associate professor at the Howard University College of Dentistry, Department of Comprehensive Care, in the Division of Periodontology. She can be reached at crystal.mcintosh@howard.edu.
Disclosure: The authors report no disclosures.



