 |
| Figure 1. The STATDDS Bruxism and Sleep Monitor (STATDDS) home test provides objective data on bruxism and obstructive sleep apnea (OSA). |
INTRODUCTION
Bruxism is one of the most common dental diseases, with one in every 3 patients coming into the office having some form of bruxism.1 Even though bruxism is so common, it is still one of the least understood dental problems. Certainly every dentist knows that bruxism is co-morbid with temporomandibular disorders (TMD), orofacial pain in the head and neck, certain headaches, and migraines. To be honest, many dental professionals just take it for granted, to the point where a treatment plan is not very thought through, beyond making the patient a “bruxism” appliance, that is.
What kind of bruxism appliance do you make in your practice? Most dentists have a favorite regardless of the intensity of the patient’s bruxism or the TMD/orofacial pain with which the patient presents. Some of you like an appliance that is an anterior bite plane, others like full-arch coverage, and some only use posterior coverage. An American Academy of Facial Esthetics (AAFE) study in September 2013 of 946 dental professionals found that most only use one type of bruxism appliance 95% of the time, regardless of the patient’s problem. Also, according to the same study, 86% of these same dentists say that the bruxism appliance does not resolve the patient’s conditions satisfactorily. Another reason that bruxism therapy has been so frustrating in the past is that there was no way to objectively measure a patient’s bruxism by monitoring the number of bruxism and clenching episodes per sleep hour.
In listening to feedback from many lecture attendees each year, I’ve found that clinicians routinely report that bruxism appliance therapy is one of the most challenging and frustrating treatments they deliver to patients. The scenario typically is this: patients present with some kind of facial pain; we tell them the pain is coming from bruxism, which happens while they sleep; we deliver an appliance and tell them to wear this for one to 3 months; and then we simply wait and see what happens. Most of the time, the patient gets worse, we adjust the appliance, and then we keep adjusting it until either we give up or the patient gives up and, worse yet, does not come back. How many times has that scenario happened to you? Let’s take a step back and examine this more closely from a few angles.
Obstructive Sleep Apnea and Bruxism: Are These Related?
First, let’s take a look at one of the possible causes of bruxism, and it will surprise many of you reading this article.
Dental sleep medicine is a fast growing area of dentistry. There are approximately 40 million people in the United States with obstructive sleep apnea (OSA), with 90% of those undiagnosed. Simply put, OSA is a medical condition in which there is a physical obstruction (tongue, pharyngeal muscles, epiglottis, vocal cords, as examples) that blocks the airway which then stops the patient from breathing during sleep. An apnea is an event where the patient stops breathing for a minimum of 10 seconds during sleep. A hypopnea is an event where the patient has significantly reduced airflow because of a partially blocked airway for at least 10 seconds while sleeping. Patients with OSA will have multiple apneas/hypopneas every night while they sleep, with the potential to severely impact their health. OSA is co-morbid, dramatically increasing the incidence and severity of diabetes, hypertension, stroke, and heart attacks in patients. (Let’s not forget that dentists are patients too, by the way.)
Okay, so we agree that OSA is a very significant health problem; why should the dental profession care? One reason is that we certainly care about our patients, and we should be screening for OSA with simple self-tests as part of a patient’s medical history. The other reason is that moderate to severe bruxism is co-morbid with OSA. What is the connection? The brain’s mechanism to get the patient to breathe when he or she has a blocked airway causing an apnea is as follows: The brain needs to open the airway and gets the muscles of mastication to start working hard and fast, a process we know as bruxism. The masticatory muscles move the jaw forward, the airway opens, and the patient takes in a deep rescue breath. Then, patient falls back asleep, the airway gets blocked again, and the process repeats itself over and over many times during the night. This is known in evidence-based studies as sleep bruxism.2,3
This same patient wakes up in the morning, the jaws hurt, the facial muscles hurt, and the patient has headaches. The individual then comes to your office because he or she has TMD, and it is clear from an examination that the patient is bruxing. If you don’t have any knowledge about OSA, or whether the exact origin of the pain is in the TM joint (TMJ) or the head and neck muscles, how would you know what kind of appliance to make? Let’s say your patient has OSA and you choose your favorite bruxism appliance, which may position the mandible posteriorly; you will hopefully realize that this “bruxism” appliance will close the patient’s airway further at night, making the OSA worse and most likely resulting in an increase in bruxism activity. Additionally, if the patient’s orofacial pain is coming from either the TMJ and/or muscle trigger points and you make the wrong kind of appliance, the pain will get worse, not better.
This is why I and the AAFE faculty all teach that there is no such thing as just making a “bruxism” appliance for patients. You need to consider all of these questions before you put an appliance in your patient’s mouth:
- Does the patient have sleep apnea?
- Does the patient have orofacial pain caused by muscles?
- Does the patient have orofacial pain originating in the TMJ?
- Does the patient have prior restorations, such as implants, veneers, crowns, bridges, and/or large restorations? (Note: This will determine appliance design.)
- Does the patient only have bruxism? If only protection of the dentition is needed with no other conditions, use the appliance of your choice.
In the past, many dentists have invested in a sleep monitor that only measures for OSA. Because OSA is a medical condition, which requires a diagnosis by a physician, and the dentist could not directly relay any kind of data regarding bruxism, these cases were handed over to the physician, who might not have been knowledgeable about dental sleep medicine or bruxism. Dentists also did not receive any information about the patient’s bruxism from these monitoring units.
New Technology
There has been an exciting advancement in the areas of bruxism and dental sleep medicine that will now let a dental clinician objectively collect data to measure bruxism and OSA in patients. The STATDDS Bruxism and Sleep Monitor (STATDDS) (Figure 1) is a very cost-effective home test device that the patient wears at night while sleeping. The exclusive software that comes with this monitor, made specifically for dentistry, analyzes the testing data and gives the dentist a simple-to-understand report with the patient’s bruxism episodes index (BEI) and the apnea/hypopnea index (AHI). The BEI measures the number of bruxism episodes per sleep hour and the AHI measures how many apnea/hypopneas per sleep hour. The monitor can be purchased, or it can also be rented by the dental practice. It is affordable, as each home test costs less than $20 to administer. Currently, this is the only monitor of its kind with specialized software that has been specifically configured to analyze both the BEI and AHI, and with the ability to produce patient specific reports for dental offices.
I use the rule of 5 when looking at these numbers: If the BEI is greater than 5, the patient has clinically significant and destructive bruxism that needs to be addressed not only with an appliance, but also in my choice of dental materials if any restorative dentistry is needed (such as crowns, bridges, implants, etc). If the AHI is higher than 5 and less than 30, then a mandibular advancement appliance for obstructive sleep apnea is now considered primary therapy. (Note: Remember that OSA is a medical condition that requires a diagnosis by a physician.) I can now show a physician that the patient has bruxism, for which I am the primary provider as a dentist and, if the sleep apnea is diagnosed as mild to moderate, I can take care of both conditions with the right appliance.
MINI CASE REPORTS
Here are some examples of how objective evidence and criteria now can help with my diagnosis and treatment plan.
 |
Case 1
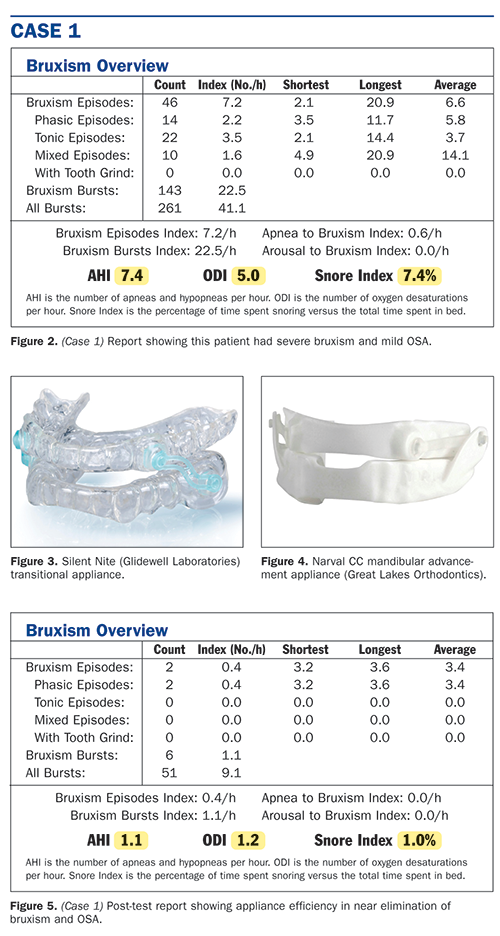
Figure 2 shows a report generated with the STATDDS monitor. This patient had a BEI of 7.2 per hour and an AHI of 7.4. This patient has severe bruxism and numbers that indicated mild OSA. A treatment plan was created with the patient’s physician. An AAFE Class I transitional appliance, such as a Silent Nite (Glidewell Laboratories) (Figure 3), was made for the patient to see if he could tolerate mandibular advancement to open his airway. This appliance eliminated his snoring, which was a good indication that further appliance therapy would most likely be effective. At this point, an AAFE Class IV mandibular repositioning appliance that has been FDA approved for OSA (such as a Narval CC [Great Lakes Orthodontics]) (Figure 4) was made for the patient. The patient was then retested with the STATDDS home test monitor while wearing the appliance and one can see the improvement in Figure 5; the patient’s BEI was much improved (at 0.4 per hour) and the AHI dropped to 1.1. We now have objective data showing the success of the mandibular repositioning appliance, resulting in the elimination of the patient’s bruxism and OSA. The patient’s physician was pleased, and the patient was very happy. Furthermore, as the treating dentist, I was assured that his dental implant therapy would last a long time because it would not be subjected to severe bruxism forces.
 |
Case 2
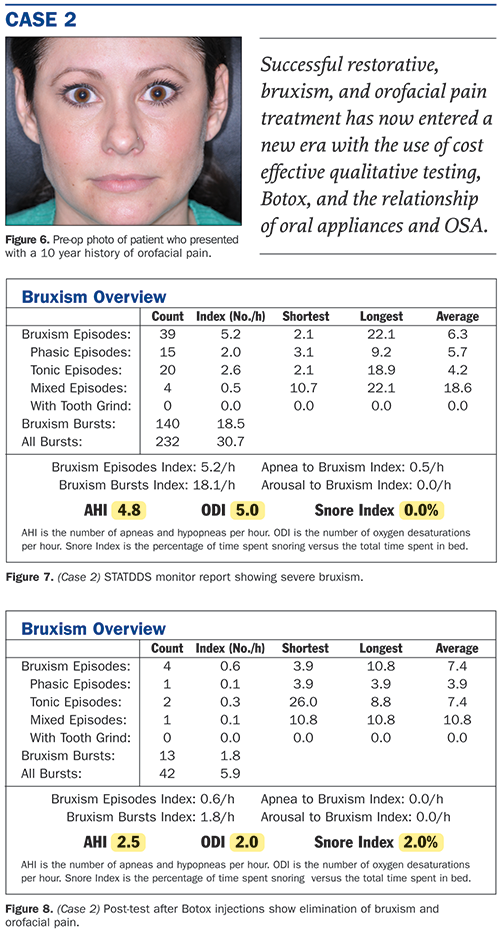
Thousands of dental professionals are now using Botox for relief of bruxism and orofacial pain. With the STATDDS monitor, we can now quantify the successful results as well as manage the dosage needed, depending on the test results. This patient is a good example of the demonstrable success that we can now measure with objective evidence.
Figure 6 shows the pre-op photo of a patient who came into the office with a 10-year history of orofacial pain. Her test results (Figure 7) showed a BEI of 5.2 and an AHI of 4.8. After trigger point injections with approximately 60 units of Botox, her postoperative test and the results were impressive (Figure 8). The patient’s BEI fell to 0.6. Interestingly, the patient’s AHI also dropped significantly. (Both the BEI and AHI results in patients are a development currently being studied by the AAFE in a multilocation study.) Figure 9 shows the patient’s aesthetic results after therapeutic injections with Botox as well as the elimination of her orofacial pain for the first time in 10 years. Cases like this clearly demonstrate to both the patient and the clinician how successful Botox therapy can be in the treatment of bruxism and orofacial pain. I use Botox routinely in most of my restorative cases to control the masticatory muscles to achieve long-term success for the dentistry I place in patients’ mouths. With the ability to now obtain objective and reliable data, I can now quantify and titrate my Botox dosages for maximum effectiveness.
 |
| Figure 9. Botox injections improved the patient’s aesthetics and also eliminated her orofacial pain. |
TRAINING IS REQUIRED
Training is essential in the areas of orofacial pain, dental and facial aesthetics, dental sleep medicine, and oral appliances for bruxism therapy before a dentist ever makes another “bruxism” appliance again. Many bruxism appliances that are currently being made may negatively impact a patient’s health if you do not understand the impact these appliances have on the TMJ, orofacial pain, and OSA. Successful restorative, bruxism, and orofacial pain treatment has now entered a new era with the use of cost effective qualitative testing, Botox, and the relationship of oral appliances and OSA. (When documented and billed properly, dentists can also often be paid by the patient’s medical insurance for many of these services.) It is time for dentistry to catch up with medicine in the ability to objectively measure and use data to help us diagnose and more effectively treatment plan our patients for the best therapeutic pain and restorative outcomes.
References
- Academy of General Dentistry. AGD: FACTSHEET. What Exactly Is Bruxism? Available at: cfdds.com/images/pdfs/bruxism.pdf. Accessed on July 24, 2014.
- Lavigne GJ1, Rompré PH, Montplaisir JY. Sleep bruxism: validity of clinical research diagnostic criteria in a controlled polysomnographic study. J Dent Res. 1996;75:546-552.
- Khoury S, Rouleau GA, Rompré PH, et al. A significant increase in breathing amplitude precedes sleep bruxism. Chest. 2008;134(2):332-337. [Epub May 19, 2008]
Further Reading and Learning Resources
The Web site facialesthetics.org offers information about live-patient frontline TMJ/orofacial pain training, frontline dental sleep medicine, bruxism therapy and medical insurance, and Botox and dermal fillers training. You can also download Dr. Malcmacher’s resource list and sign up for a free monthly e-newsletter at the site.
Dr. Malcmacher is a practicing general dentist and an internationally known lecturer and author. He is president of the American Academy of Facial Esthetics. He also has been awarded his Mastership in the AGD. He can be reached at (800) 952-0521 or via e-mail at the address drlouis@facialesthetics.org.
Disclosure: Dr. Malcmacher is president of the American Academy of Facial Esthetics and is a consultant for STATDDS.











